[ad_1]
While type 2 diabetes is largely preventable, type 1 diabetes is a disruptive autoimmune disease that has been once thought incurable. “Once” is the key word here, because a new and uncontroversial form of stem cell therapy should be able to cure the disease once and for all.
Relying on the transformation of a small piece of adult skin tissue into beta cells in the pancreas – the ones that produce the illusory hormone insulin in diabetics – the treatment bypasses the genetic mutation that causes the immune system to attack these cells that create disease.
Diabetes, especially type 1, severely limits quality of life and, if not carefully managed, can lead to serious complications such as foot amputations and early mortality.
In addition, it costs the US healthcare industry approximately $ 85,000 per patient per lifetime treatment, a tremendous burden that, if removed, could save the industry in the hundreds of millions.
Researchers at the Salk Institute for Biological Studies, a pioneering force in all forms of biology, pioneered a new way to produce beta-pancreas cells for this type 1 treatment – and now the only thing that precludes its availability in hospitals are safety trials in humans.
“Stem cells are an extremely promising approach for developing many cell therapies, including better treatments for type 1 diabetes,” Salk professor Juan Carlos Izpisua Belmonte, lead author of the corresponding article, told the department. release from Salk.
“This method of making large numbers of safe and functional beta cells is an important step forward.”
CHECK: Enthusiastic Scientists Make Breakthrough in Type 2 Diabetes with First-Ever Insight into How Disease-causing Proteins Work
The reason the stipulation is important is that although their article gives 11 quotes to the concept of using stem cell therapy to cure diabetes, dating back to 2007, there are still insurmountable challenges with cell manufacturing. beta-pancreas.
Cultivate a cure
Prior to the use of stem cells, patients could receive islet of Langerhans cells transplanted from donors with fully functioning insulin systems, but low donor levels made this treatment a slow burner, even if ‘he succeeded.
Existing stem cell methods only successfully convert about 10-40% of human pluripotent stem cells (PSCs) into beta-pancreatic cells. In addition, PSC beta-pancreas cells tend to be heterogeneous and contain unwanted cell types that can hinder or disrupt the maturation and function of the desired beta-pancreas cells.
Previous methods of using CSPs to create beta cells sometimes lead to dysfunction or, in some cases, the formation of teratomas (sometimes huge) or cysts.
AFTER: No more needles: Scientists launch first-of-its-kind blood sugar test for pain-free delivery to diabetics
“In order for beta cell treatments to eventually become a viable option for patients, it is important to make these cells easier to manufacture,” co-lead author Haisong Liu, former member of the lab’s lab, told Salk. Dr Belmonte. “We have to find a way to optimize the process.
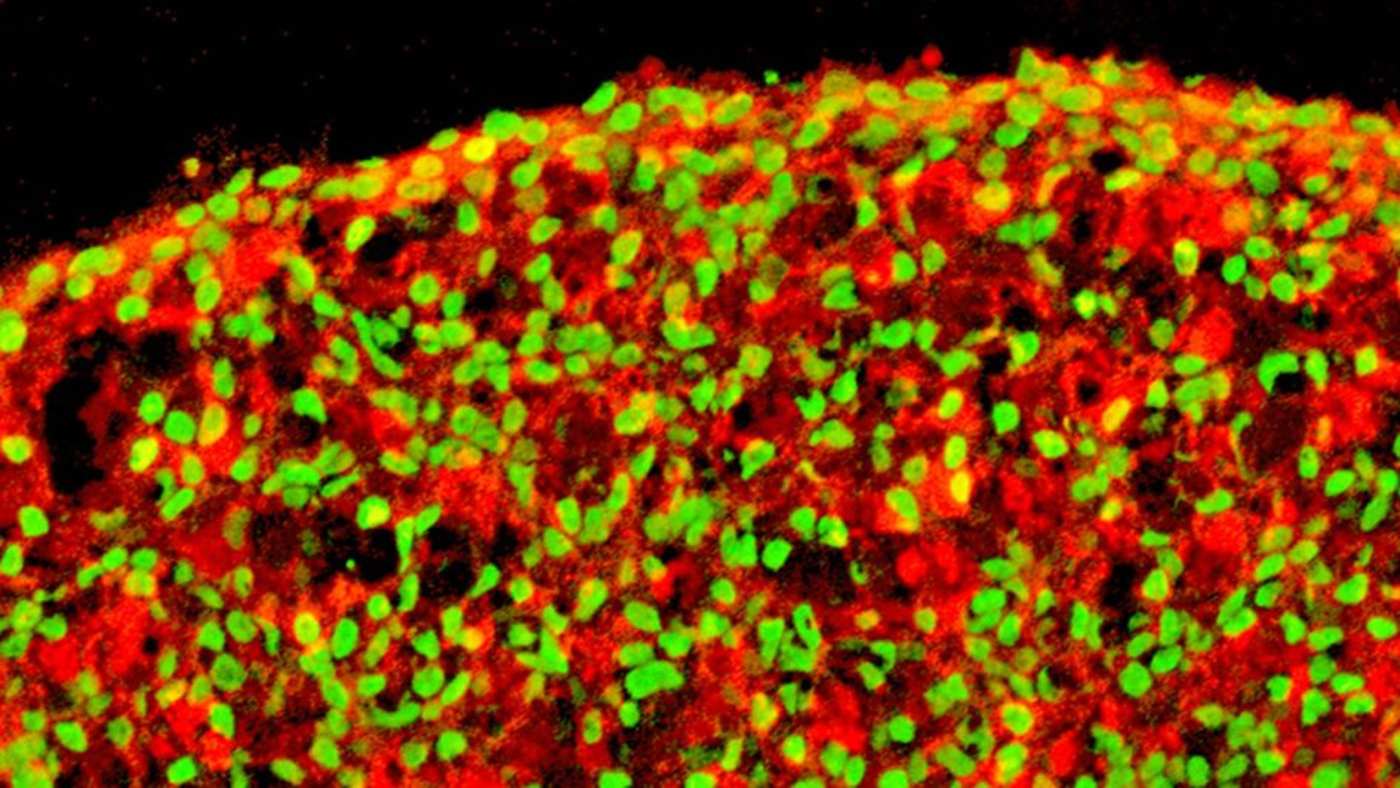
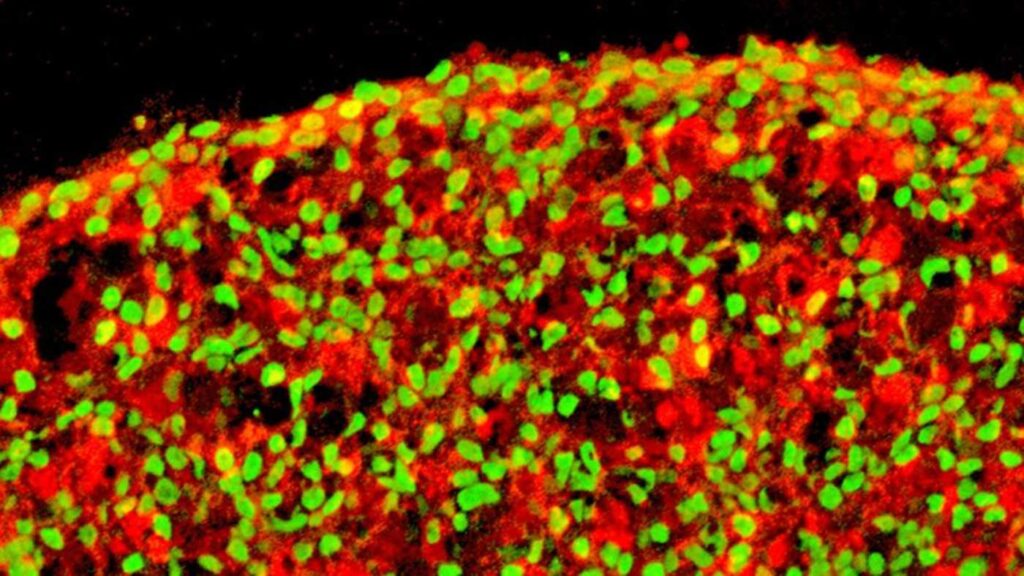
And that’s exactly what they did. Using a 3-dimensional petri dish allowed cells to interact and grow in an environment similar to what they would naturally have, and within two weeks of transplantation in diabetic mice, their blood sugar levels. fell to normal levels like those seen in non-diabetic mice. .
RELATED: Walmart Unveils Inexpensive Insulin For Diabetes Patients Who Cannot Afford It Easily
To test the safety and effectiveness of the manufactured beta cells, the team transplanted them at different stages and observed the effects. At the highest stages of growth, cells did not cause cysts to form even 20 weeks after implantation and exhibited proper functionality. in vivo and in vitro.
The three-dimensional stem cell production method will continue to be refined at Salk, with the only human trials remaining and FDA approval. At least one pharmaceutical company has already jumped into trials this year to test stem cell therapy for type 1 diabetes, so it seems the days of the disease are numbered.
SHARE this hopeful research with friends on social media …
[ad_2]
Source link