[ad_1]
Researchers at MIT and the Dana-Farber Cancer Institute have developed a new way to determine whether or not individual patients will respond to a specific cancer drug. This type of test could help doctors choose alternative therapies for patients who do not respond to therapies normally used to treat their cancer.
The new technique, which involves removing tumor cells from patients, treating the cells with a drug, and then measuring changes in cell mass, could be applied to a wide variety of cancers and drug treatments, says Scott Manalis , Research Director David H. Koch Professor of Engineering in the Departments of Biological and Mechanical Engineering, and Member of the Koch Institute for Integrative Cancer Research.
“Essentially, all anticancer drugs used clinically directly or indirectly stop the growth of cancer cells,” Manalis explains. “This is why we believe that measuring mass could offer a universal reading of the effects of many different types of drug mechanisms. “
The new study, which focused on glioblastoma, an aggressive form of brain cancer, is part of a collaboration between the Koch Institute and the Dana-Farber Precision Medicine Programs to find new biomarkers and diagnostic tests cancer.
Manalis and Keith Ligon, director of the Center for Patient Derived Models at Dana-Farber and associate professor at Harvard Medical School, are the lead authors of the study, which appears today in Cell reports. The main authors of the article are Max Stockslager SM ’17, PhD ’20 and Dana-Farber research technician Seth Malinowski.
Measuring cancer cells
Glioblastoma, diagnosed in about 13,000 Americans a year, is incurable, but radiation therapy and drug treatment can help extend the expected lifespan of patients. Most do not survive more than one to two years.
“With this disease, you don’t have a lot of time to make adjustments. So if you take an ineffective drug for six months, that’s pretty big, ”Ligon says. “This type of test could help speed up the learning process for each patient and aid in decision making.”
Patients diagnosed with glioblastoma usually receive a chemotherapy drug called temozolomide (TMZ). However, this drug only helps about 50 percent of patients.
Currently, doctors can use a genetic marker – methylation of a gene called MGMT – to predict whether patients will respond to TMZ treatment. Patients who have this marker generally respond better to the drug. However, the marker does not offer reliable predictions for all patients due to other genetic factors. For patients who don’t respond to TMZ, there are a handful of alternative drugs available, Ligon says, or patients can choose to participate in a clinical trial.
In recent years, Manalis and Ligon have been working on a new approach to predict patient responses, based on measuring tumor cell response to treatment, rather than on genomic signatures. This approach is known as precision functional medicine.
“The idea behind Precision Functional Medicine is that for cancer, you can take a patient’s tumor cells, give them the drugs the patient might receive, and predict what would happen before you give them to the patient.” , explains Ligon.
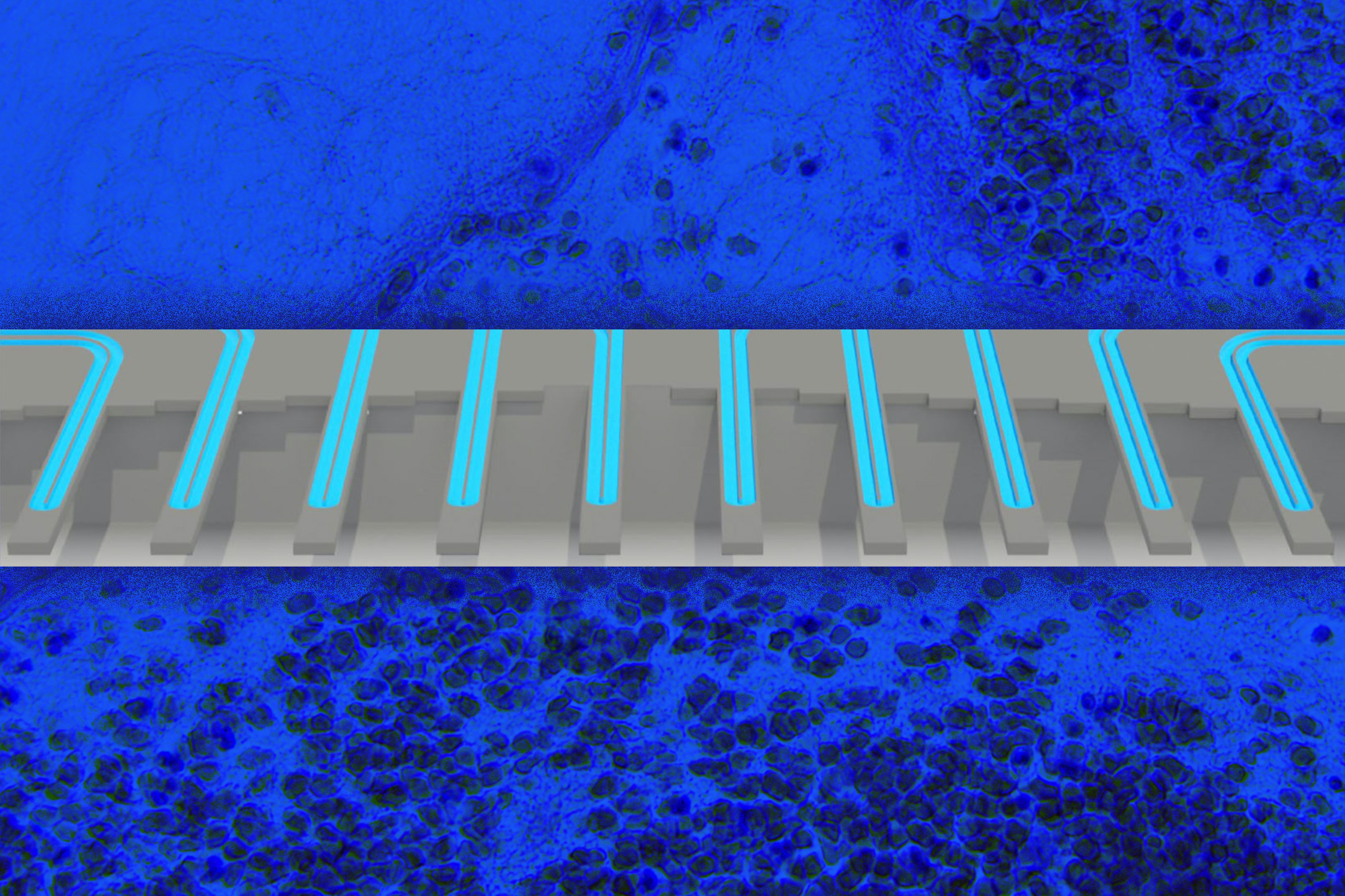
Scientists are working on many different approaches to precision functional medicine, and one technique Manalis and Ligon have followed is to measure changes in cell mass that occur after drug treatment. The approach is based on a technology developed by the Manalis laboratory to weigh individual cells with extremely high precision by passing them through vibrating microchannels.
Several years ago, Manalis, Ligon and their colleagues demonstrated that they could use this technology to analyze how two types of cancer, glioblastoma and acute lymphoblastic leukemia, respond to treatment. This result was based on measuring individual cells multiple times after drug treatment, allowing researchers to calculate how their growth rate changed over time after treatment. They showed that this statistic, which they called the mass accumulation rate (MAR), was strongly predictive of the sensitivity of cells to a given drug.
Using a high-throughput version of this system, which they developed in 2016, they were able to calculate an accurate MAR using just 100 cells per patient. However, a disadvantage of the MAR technique is that the cells must remain in the system for several hours, so that they can be weighed repeatedly, in order to calculate the rate of growth over time.
In their new study, the researchers decided to see whether a simpler and significantly faster approach – measuring the subtle changes in unicellular mass distributions between treated and untreated cancer cells – would be able to predict patient survival. They performed a retrospective study with a set of live glioblastoma tumor cells from 69 patients, donated to the Ligon lab and the Dana-Farber Center for Patient Derived Models, and used them to grow spheroid tissue cultures. After separating the cells, the researchers treated them with TMZ and then measured their mass a few days later.
They found that by simply measuring the difference in mass between cells before and after treatment, using as little as 2,000 cells per patient sample, they could accurately predict whether the patient had responded to TMZ or not.
Better predictions
The researchers showed their mass measurement to be just as accurate as the MGMT methylation marker, but the mass measurement has an added advantage in that it can work in patients for whom the genetic marker does not reveal sensitivity. at TMZ. For many other types of cancer, there are no biomarkers that can be used to predict response to drugs.
“Most cancers don’t have a genomic marker that can be used at all. What we are arguing is that this functional approach could work in other situations where you have no option of a genomic marker, ”explains Manalis.
Since the test works by measuring changes in mass, it can be used to observe the effects of many different types of cancer drugs, regardless of their mechanism of action. TMZ works by stopping the cell cycle causing cells to get bigger because they can’t divide anymore but still increase in mass. Other cancer drugs work by interfering with cell metabolism or damaging their structure, which also affects cell mass.
The researchers’ long-term hope is that this approach can be used to test several different drugs on an individual patient’s cells, in order to predict which treatment would work best for that patient.
“Ideally, we would test which drug the patient was most likely to get, but we would also test things that would make up the back-up plan: first-, second-, and third-line therapies, or different combinations of drugs,” Ligon explains. , who is also chief of neuropathology at Brigham and Women’s Hospital and pathology consultant at Boston Children’s Hospital.
Manalis and Ligon co-founded a company called Travera, which licensed this technology and now collects data from patient samples from several types of cancer, in hopes of developing clinically validated laboratory tests that can be used to help patients.
The research was funded by the MIT Center for Precision Cancer Medicine, the DFCI Center for Patient Derived Models, the National Cancer Institute’s Cancer Systems Biology Consortium, and the National Cancer Institute’s Koch Institute Support (core) grant.
[ad_2]
Source link