[ad_1]
Charles Beschta had heartburn and his breathing became so difficult that he had to stop singing in his choir.
Then he had pneumonia. While working in the welding industry, he began to lose all his potential.
The doctors diagnosed him with systemic scleroderma, an autoimmune disease that hardens the skin and tissues of the internal organs – in the case of Beschta, mainly the lungs and the digestive tract.

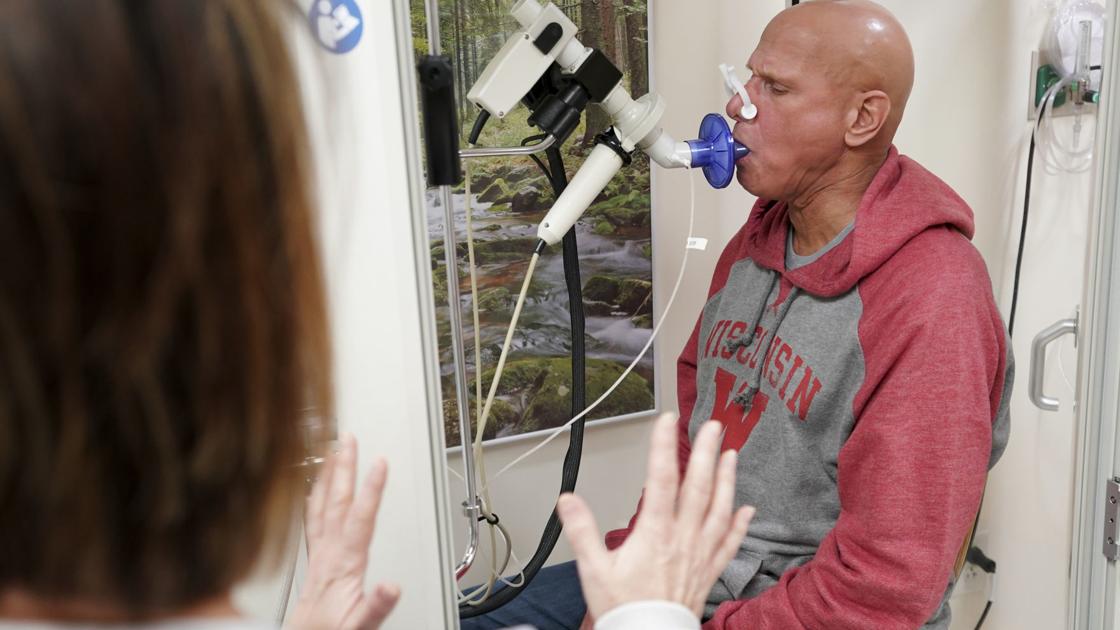
Charles Beschta is resting at UW Hospital last week while undergoing a pulmonary function test, administered by respiratory therapist Lora Mercier. The test requires that people inhale deeply and exhale thoroughly several times, which is particularly difficult for people suffering from lung disease, such as Beschta. "We did not feel as bad as in the past," said Beschta, who had a stem cell transplant in early April for severe scleroderma, an autoimmune disease.
Medications can help, but there is no cure. With severe cases like Beschta, about half of patients die within 10 years, said Dr. Kevin McKown, his rheumatologist at UW Health.
McKown proposed another treatment: a stem cell transplant, which Beschta received at UW Hospital in early April. He is the first patient to undergo the scleroderma treatment procedure at UW, after a national study last year showed that it worked better than drugs.
"I really hope things will get better," said Beschta, 55, who lives near Bonduel, between Wausau and Green Bay, during a follow-up visit to the hospital last week. "I pray that's the cure."
Stem cell transplants, also called bone marrow transplants, are typically used to treat certain cancers. Under conditions such as scleroderma, in which the immune system attacks its own tissues, the goal is to eliminate the defective immune system and reconstitute it with a new one.
First, doctors take blood from the patient and isolate the stem cells. Then, the patient receives chemotherapy and radiation therapy to eradicate the immune system. The stem cells are then infused to grow new immune cells.
In the national study, 79% of patients with severe scleroderma who had a transplant were alive without serious complications after four and a half years, compared with 50% on medication.
"There was a quick consensus that this should be the standard of care," McKown said. For patients like Beschta, "maybe it gives the immune system a chance to reset itself".
The medical school in Wisconsin, near Milwaukee, did one of the transplants in 2010 as part of the study, but has not done so since, said Dr. Rheumatologist Dr. Mary Ellen Csuka. The patient is fine today, said Csuka.
As in the national study, UW Hospital has taken a step further to purify Beschta stem cells. The cells were labeled with magnetic beads and passed through a machine that collected stem cells and removed others, such as T cells that could cause problems, said Dr. Peiman Hematti, who directs the laboratory involved.
McKown said it could take two years to evaluate the effectiveness of the Beschta transplant, but Beschta said last week that he was feeling better. "My energy level seems to be getting stronger," he said.
A former sailor who worked at Miller Electric in Appleton for more than 30 years, Beschta developed acid reflux several years ago. At about the same time, his breathing became laborious. Diagnosed with asthma, he began using inhalers.

Charles and Linda Beschta, who live near Bonduel in Shawano County, said their lives had been greatly affected by his severe scleroderma, which he had been diagnosed last year. The couple, who has two children aged 21 and 19 and a 2-year-old grandson, said that his community had been supportive. A recent event raised funds to cover travel expenses, lost wages due to absences from work, and unpaid medical expenses.
In June 2017, he had pneumonia. At the beginning of last year, at UW Hospital, he was diagnosed with severe scleroderma.
The disease has caused the formation of calcium deposits on the skin and on many parts of his body. "It looked like he had ringworm," said his wife, Linda Beschta.
His esophagus became so scarred that he had to undergo surgery to clean it up and be able to eat. He had significant digestive discomfort, including frequent bowel movements, forcing him to stop eating fresh vegetables.
At work, he had to wear gloves to seize the reels around which he wrapped the thread. He was so exhausted that he often took a nap instead of eating during the lunch break.
Beschta initially stated that he was reluctant to undergo stem cell transplant, which could put his life in danger.
But when he heard about the results of the national study, he felt compelled to try it.
"My chances have increased dramatically and for me it was enough," he said.
[ad_2]
Source link