[ad_1]
We call for a worldwide moratorium on all clinical uses of germ line modification in humans, that is to say the modification of hereditary DNA (in sperm, ova or embryos) to make them genetically modified children.
By "global moratorium" we do not mean a permanent ban. On the contrary, we call for the establishment of an international framework in which nations, while retaining the right to make their own decisions, voluntarily undertake not to endorse the use of the Germ line clinical edition unless certain conditions are met.
For starters, there should be a fixed period during which no clinical use of germ line modification is allowed. In addition to allowing for discussion of the technical, scientific, medical, social, ethical and moral issues to be considered before any change in the germ line, this period would provide the time needed to establish an international framework.
Subsequently, nations may choose to follow separate paths. At present, about 30 countries have legislation that directly or indirectly prohibits all clinical uses of germ line modification.1and they could choose to maintain the moratorium indefinitely or apply a permanent ban. However, any country may also choose to allow specific applications of germ line editing, provided that it begins with: publicly notifying its intention to review the application and engage for a fixed period of international consultations on the desirability of doing so; determines by transparent evaluation that the request is justified; and ensures that there is a broad consensus of society in the country on the relevance of the application. Nations might well choose different ways, but they would agree to proceed openly and with respect for the views of humanity on an issue that will ultimately affect the entire species.
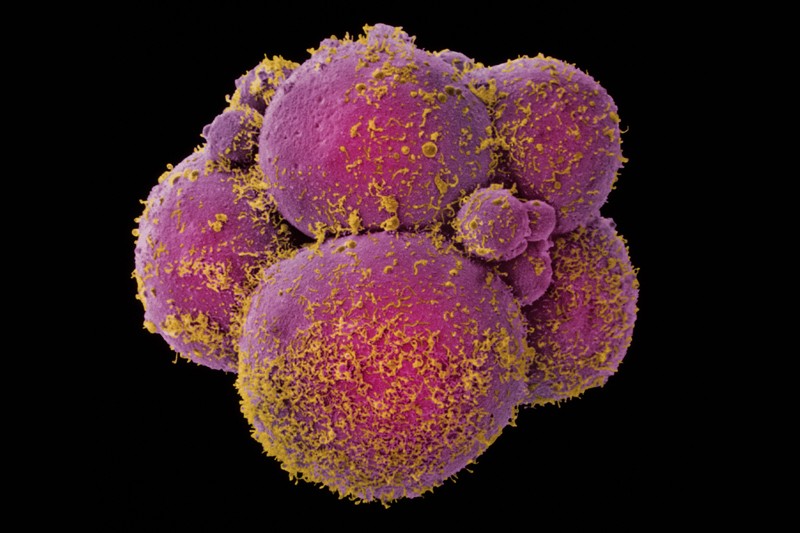
Let us be clear, our proposed moratorium does not apply to germ line modification for research purposes, provided that these studies do not involve the transfer of an embryo to a person's uterus. This does not apply either to the editing of the genome in human somatic cells (non-reproductive) to treat diseases, for which patients can give informed consent and modifications of DNA are not heritable.
Among the 18 signatories of this call are scientists and ethicists citizens of 7 countries. Many of us have been involved in the field of gene editing by developing and applying technology, organizing and speaking at international summits, serving on national advisory committees and by studying the ethical issues raised.
We explain here why we think that such a moratorium is now justified and illustrate the possible functioning of an international framework.
The need
At the first International Summit on the Modification of the Human Gene in December 2015, the organizing committee issued a statement on the appropriate uses of technology (see go.nature.com/2erqwpc). Regarding the issue of the manufacture of genetically modified children, he concluded that "it would be irresponsible to proceed with any clinical use … until and until (i) safety concerns are met. and effectiveness have been solved … and (ii) there is a broad consensus of society the adequacy of the proposed application.
This should have been understood to mean that the clinical uses of germ line modification should not yet occur elsewhere in the world. Yet later events suggest that this statement was inadequate.
First, in China, the biophysicist He Jiankui has published embryos to create at least two babies. Secondly, scientists who were apparently aware of this work did not take adequate measures to prevent it. Third, there is growing interest in proposals for genetic improvement of human beings.2,3. Fourth, some commentators have interpreted subsequent statements as weakening the need for broad social consensus.4; these statements include a report from the 2017 National Academies of Science, Engineering and Medicine of the United States5 and a 2018 statement from the organizing committee following the second International Summit on Human Genome Modification (see go.nature.com/2rowv3g). Finally, no mechanism has been established in the coming years to ensure an international dialogue on whether, and if so, when, the clinical edition of germ line might be appropriate.
A global moratorium and framework is therefore needed to ensure adequate consideration of issues related to the clinical uses of germ line modification.
Technical considerations In order for germline modification to even be considered for clinical application, its safety and efficacy must be sufficient – taking into account unmet medical needs, potential risks and benefits, as well as the existence of alternative approaches. alternatives.
Although the techniques have improved in recent years, germ line modification is not yet sufficiently safe or effective to warrant clinical use. As was evident at the second summit, the scientific community agrees that, for clinical germ line editing, the risk of not making the desired change or introducing mutations unintentional (non-targeted effects) is always too high. Considerable research is being conducted on this issue.
Scientific considerations. No clinical application of germ line modification should be considered if its long-term biological consequences are not sufficiently understood – both for individuals and for the human species.
Among the wide range of possible genetic modifications, it is useful to distinguish between "genetic correction" and "genetic improvement".
By genetic correction we mean to edit a rare mutation that has a high probability (penetrance) of causing a single gene serious disease, in order to convert the mutation into a DNA sequence carried by most people. Assuming that this can be done without errors or untargeted effects, genetic correction could have a predictable and beneficial effect.
Genetic improvement, on the other hand, involves much broader efforts to "improve" individuals and species. The possibilities range from attempting to change the risk of a common disease by replacing particular genetic variants with alternative variants existing in the human population, integrating new instructions into a person's genome to improve, for example, example, its memory or its muscles, or even new biological functions, such as the ability to see infrared light or to eliminate certain toxins.
Understanding the effects of any proposed genetic improvement will require further study – including the genetics of the human population and molecular physiology. Even in this case, substantial uncertainty would probably remain.
Changing the risk of disease by replacing genetic variants with variants is a daunting task, since variants that reduce the risk of certain diseases often increase the risk of others. A common variant in the gene SLC39A8for example, reduces the risk of developing hypertension and Parkinson's disease, but increases the risk of developing schizophrenia, Crohn's disease and obesity6. Its influence on many other diseases – and its interactions with other genes and with the environment – remains unknown.
It will be much more difficult to predict the effects of completely new genetic instructions – not to mention how many changes will interact when they occur simultaneously in future generations. Attempting to reshape the species based on our current knowledge would be a pride.
The work of He illustrates this point. Seeking to reduce the risk of contracting AIDS in children if he was exposed to HIV later in life, he tried to inactivate the gene CCR5which encodes a receptor used by HIV to enter the cells. However, this change is not benign: it has been reported to significantly increase the risk of complications and death due to some other viral infections, including West Nile virus and influenza. It could also have other consequences – positive and negative (see Nature http://doi.org/gfphqv (2018) and ref. 7). As a societal solution to AIDS, disrupt CCR5 the clinical edition of germ line is misguided. The modification of the germ line would not help the infected people today and it would take several decades of widespread use to reduce the epidemic. In addition, if an effective HIV vaccine were developed, genetic improvement would not confer any benefit on AIDS, but would increase the risk of complications from other infections.
Medical considerations. Clinical application should only be considered if there is a sufficiently compelling reason. At the very beginning of new technologies, the bar should be high.
Any genetic improvement would be unjustifiable at this stage, given the scientific considerations already mentioned. The issue of genetic correction is more complex.
Some argue, especially in the popular press, that it is urgent to develop a germ line to prevent children from being born with a serious genetic disease. However, couples who know they are at risk of transmitting a serious disease-causing mutation already have a sure way of not doing so. They can use in vitro fertilization (IVF) in conjunction with preimplantation genetic testing (PGT), prenatal testing, sperm donors, egg donors, embryo donors or adoption. In particular, the use of IVF followed by genetic screening of embryos to ensure that only those unaffected are transferred into the person's uterus ensures that the couple will not have children with the disease genetic.
The real problem is that most children with serious genetic diseases are born to couples who did not know they were at risk. Systematic access to genetic testing prior to conception could allow most couples at risk to use the current options, if they wish. Better access to neonatal screening is also needed to ensure that babies with a genetic disease can receive any available treatment immediately.
What is the role of genetic correction? Although IVF coupled with GPT can ensure that couples with a serious disease-causing mutation will not have an affected child, it does not always give a baby.
In most cases, the problem arises from the limitations of the process, related to the number and quality of the eggs harvested, as well as the growth and implantation of the embryos produced. IVF itself does not always succeed; the transfer of an embryo leads to a successful pregnancy in about 30% of cases in women under 35 years and in less than 10% of cases in women over 40 years. TCP reduces the number of embryos available for transfer because some embryos are rejected as such. result of genetic test results, and others fail to develop in vitro at a stage and quality that makes them fit for testing.
In most cases, appropriate embryos are available for transfer after a TCP. However, when only a few are available to begin, there may be none after the test. Couples can repeat the process and succeed in subsequent trials, but some may never get unaffected embryos.
It has been suggested that if germ line modification is very effective and safe, it could increase the proportion of couples who have had a pregnancy. However, continuing to improve the efficiency of the IVF and PGT processes could be a better, safer, cheaper and more widely applicable solution.
At present, it is difficult to evaluate the usefulness of germ line editing to improve the efficacy of IVF coupled with CPT. The extent to which PGT decreases the effectiveness of IVF depending on the IVF protocol, the age of the mother, the number of eggs harvested and the proportion of affected embryos has not been the subject of in-depth studies. (We know only one study addressing some of these issues in a unique context.8.) The effectiveness of germ line modification is also unclear, particularly because of the need to evaluate the accuracy of embryo modification. Once these questions are clarified, the case can be weighed.
For a tiny fraction of couples, the situation is different. IVF associated with TGP alone will never help these couples because 100% of their embryos will be affected. In these cases, one of the parents is homozygous for a dominant disease or both parents are homozygous for a recessive disease. These cases are extremely rare and concern only a small minority of genetic diseases and mainly in situations where a disease allele is present at a high frequency in a population.
These rare couples may be the strongest case for a germline clinical edition, as technology is the only way to conceive unaffected children biologically related to both parents. Companies will have to weigh the legitimate interests of these couples against other issues.
Societal, ethical and moral considerations. Notwithstanding all of the above, germline clinical editing should not be used for any application without a broad societal consensus on the desirability of modifying a fundamental aspect of humanity for a particular purpose. Unless there is a wide range of voices committed equitably from the beginning, the efforts will lack legitimacy and may turn against them.
The societal impacts of clinical germ line editing could be considerable. People with genetic differences or disabilities may experience stigma and discrimination. Parents could be subject to strong peer pressure and marketing to improve their children. Children with modified DNA could be psychologically affected in a prejudicial way. Many religious groups and others will probably find the idea of reshaping the fundamental biology of the human being morally disturbing. Unequal access to technology could increase inequality. Genetic improvement could even divide humans into subspecies.
In addition, the introduction of genetic modifications in future generations could have permanent and possibly harmful effects on the species. These mutations can only be removed from the gene pool if all carriers agree to forego having children or to use genetic procedures to ensure that they do not transmit the mutation to their children.
The framework
Decisions about the clinical modification of the germ line – whether it is allowed or not, and judgments about particular applications – will take place over several decades. Because this has implications for the entire case, decisions must be informed by diverse interests and perspectives.
At this point, no results should be excluded. The world might conclude that the clinical use of germ line modification is a line that should not be crossed for any reason. By the way, some companies could support genetic correction for couples having no other way to have biologically related children, but draw a line for all forms of genetic improvement. Or, companies may one day approve the limited or widespread use of the improvement.
These decisions should not be made by individual actors – neither by scientists, doctors, hospitals or companies, nor by the scientific or medical community as a whole. Indeed, some commentators have expressed concern that the assessment processes were over-controlled by scientists and physicians.9.
What could an international framework look like?
We do not think that a purely regulatory approach will suffice because it can not deal with many fundamental issues. Regulatory agencies have narrow mandates: they are usually charged with evaluating the safety and efficacy of a new treatment, and not knowing how appropriate it is to # 39; use.
Nor are we in favor of an international treaty that would prohibit all clinical uses of germ line modification, subject to a mechanism to lift the ban for specific applications. International bans have been useful for some technologies, including nuclear, chemical and biological weapons. But the approach is too rigid for clinical germ line editing. Indeed, the United Nations Educational, Scientific and Cultural Organization (UNESCO) has endeavored to create a legally binding convention banning human cloning. This is partly explained by the difficulty of reaching agreement on the rules governing reproductive cloning to create a child, as opposed to therapeutic cloning to create a biologically compatible tissue to treat an existing person.ten.
Instead, we believe that every country should voluntarily commit to allowing no application of germ line modification unless certain conditions are met. We describe a possible approach for illustration.
The engagements
Governments would publicly declare that they would not allow any clinical use of human germ line verification for an initial period of a specified duration. Five years might be fine.
Subsequently, a nation could choose to allow a particular application, but only after. First, give public notice (perhaps two years) of its intention to consider permitting enforcement and engage in a lively international discussion on the pros and cons of such a request. Secondly, determine, by carefully and transparently assessing technical, scientific and medical considerations and societal, ethical and moral issues, that, in his opinion, the request is justified. Third, determine that there is a broad social consensus in the country on whether to proceed with editing the human germ line and the merits of the proposed application.
We are particularly attentive to the challenge of assessing the social consensus11. To be clear, the concept does not mean unanimity or the simple majority12. Society's consensus on germ line modification is something that must be judged by national authorities, just as governments make political decisions about their citizens' views on other complex social issues. A useful approach to consider is the global observatory project for genome editing.9,13,14, a network of organizations and individuals to follow the evolution of the situation and facilitate public conversations, both within nations and cultures.
A coordinating body should be set up to support the framework. This group could convene both ongoing discussions and specific consultations once a country has publicly announced that it intended to allow a particular application. The coordinating body could be organized under the aegis of the World Health Organization (WHO) or constitute a new entity through the collaborative efforts of a group of diverse nations.
The coordinating body should establish an international group to provide countries with clear, comprehensive and objective information on relevant issues by publishing reports on a regular basis (perhaps every two years). International conventions commonly use these groups to assess complex scientific and societal issues, such as fissile material, forests, natural disasters, biodiversity and climate change. We would prefer to have two distinct subgroups – one mainly composed of biomedical specialists for technical, scientific and medical considerations, and the other composed mainly of specialists in social, ethical and moral issues.
Various aspects of the framework should be specified by groups with an appropriate international reputation. The WHO and several national academies have announced their intention to convene international committees on the clinical editing of germ lines; these groups might choose to assume this task. But it is essential to include people with perspectives other than science and medicine, including people with disabilities, patients and their families, economically disadvantaged communities, historically marginalized groups, religious groups, and civil society in general. .
The justification
Some might criticize the framework we describe here because the commitment is voluntary rather than a formal treaty. However, we believe that this approach would be effective as it would encourage countries to commit to transparency, public participation, international consultation and policing within their borders. It would also give other nations the opportunity to dissuade a country from poorly designed uses. And this would provide a mechanism for countries signaling refusal that refuse to commit – or respect – those obligations that they have imposed themselves.
The governance model that we present will intentionally leave a margin for nations to adopt different approaches and come to different conclusions, informed by their history, culture, values and political systems. Nevertheless, the common principle would be that all nations agree to proceed in a deliberate manner and with respect for the views of humanity.
In addition to asking nations to take action, we ask stakeholders – including fertility clinics, hospitals, medical schools, biomedical research institutes and professional associations, as well as researchers and doctors working in the field – to publicly pledge not to engage clinical lineage editing without notice, full transparency and national approval under all relevant laws and regulations, and notification of unsanctioned efforts of which they are aware.
We recognize that a moratorium is not free. Although each nation may decide to proceed with a particular application, the obligation to explain to the world why it considers that its decision is appropriate will take time and effort.
Admittedly, the framework we are demanding will place significant speed bumps in front of the most daring projects to reconfigure the human species. But the risks of the alternative – which include harming patients and eroding public confidence – are far worse.
[ad_2]
Source link