
[ad_1]
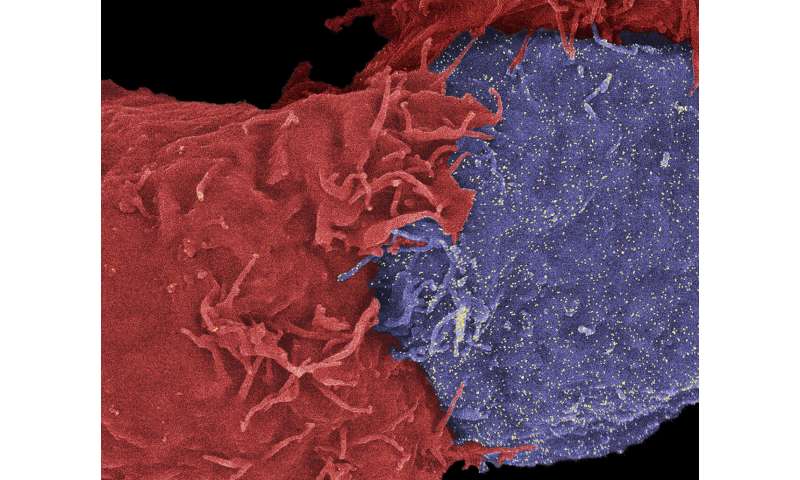
Work has focused on patients treated with immune checkpoint inhibitors, a therapy that disrupts the ability of cancer cells to "hide", allowing the body's immune cells to target and destroy tumors. (In the photo, a natural killer cell (red) attacking a cancer cell (blue) Credit: Dan Davis
Cancer patients undergoing immunotherapy are less well treated if they have recently taken antibiotics, their response and overall survival rate "collapsed".
The findings come from a study of nearly 200 cancer patients in the UK taking a type of immunotherapy called checkpoint inhibitors, which is part of the standard treatment pathway for cancer patients under NHS.
The researchers found that patients who received broad-spectrum antibiotics in the month prior to the start of treatment had a significantly poorer response to immunotherapy.
Compared to patients who received antibiotics with or without immunotherapy, antibiotic treatment prior to immunotherapy was associated with lower overall survival rates and patients' cancers were more likely to progress.
The researchers suggest that this could be due to the fact that antibiotics disrupt the balance of bacteria and microbes in the intestine, called the microbiome, which has an impact on the immune system.
The prospective study, conducted by researchers at Imperial College London and published today in the journal JAMA Oncology, emphasizes the importance of the timing of antibiotic treatment and the need to continue studies to understand the mechanisms involved.
The researchers say the findings could influence clinical practice, including a higher threshold for giving antibiotics to cancer patients starting immunotherapy.
Dr. David Pinato, of the Imperial Department of Surgery and Cancer and corresponding author of the study, said: "Cancer immunotherapy may be effective in approximately 20% of patients, but it is very difficult to predict who will respond to it: evidence that antibiotics have an impact We have shown that with prior exposure to antibiotics, patients' response to immunotherapy and survival was deteriorating. "
Immune response
As part of the study, the team examined 196 patients receiving immunotherapy as part of their routine care on the NHS, and treated at the NHS Trusts of Imperial College Healthcare and Chelsea and Westminster Hospital.
The main disease patients included non-small cell lung cancer, melanoma, head and neck cancer, carcinomas and other types of cancer. All patients have been treated with immune checkpoint inhibitors, a therapy that prevents cancer cells from "hiding", allowing the body's immune cells to target and destroy tumors.
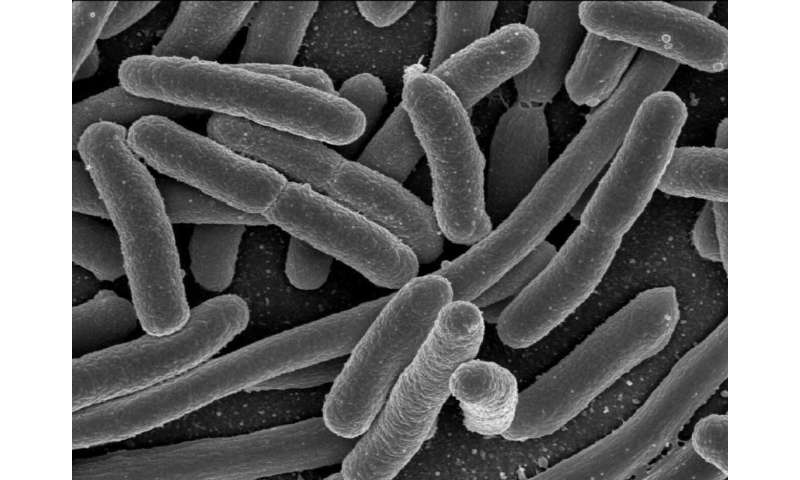
Researchers believe that broad-spectrum antibiotics before cancer immunotherapy disrupt the balance of microbes in the gut – collectively called the microbiome – reducing the diversity of insects present and potentially affecting the body's immune response. The photo shows E. coli rod-shaped bacteria, which are part of the intestinal microbiome. Credit: NIAID / NIH
The researchers looked at whether patients had received broad-spectrum antibiotics up to 30 days before starting their immunotherapy treatment, or whether they had received antibiotics during their treatment – respiratory infections being the most common cause of prescription of antibiotics.
A total of 26 patients received previous antibiotics and 68 during their immunotherapy, and the median overall survival after treatment was 14.6 months.
However, the analysis revealed that patients who had previously used antibiotics had a median overall survival of only two months, compared with 26 months for those who had not used antibiotics before treatment. A similar effect has been observed for all types of cancer.
Patients who had used antibiotics were probably less sensitive to immunotherapy, their main disease being almost twice as likely to progress. The study also showed that the effect was independent of the class of antibiotic used – which, for this group of patients, included beta-lactams, quinolones, macrolides, sulfonamides, tetracyclines, aminoglycosides and nitroimidazole.
Critical Timing
According to the researchers, it is urgent to continue work to understand the mechanism behind the reduction of the response and the decline in overall survival.
But they believe that broad-spectrum antibiotics before immunotherapy disrupt the balance of microbes in the gut, collectively called the microbiome, thereby reducing the diversity of insects present and potentially affecting the body's immune response.
"We know that the administration of antibiotics to patients affects their microbiome and more and more, the evidence shows that this affects the outcome of treatment," added Dr. Pinato.
"It's important that patients who need antibiotics to treat bacterial infections receive the medications they need," he explained. "But these results call for more and more attention in the decision-making process of some patients.
This raises the question of whether we need a higher threshold for the prescription of antibiotics in cancer patients because of immunotherapy. "
The team highlighted some limitations to the results, including the small number of patients and the lack of direct observations of changes in the gut microbiome. They also add that it's not possible to fully account for the impact that any other health problem that patients might have (comorbidities) could have had on their survival. However, they explain that they remain confident in the link and the need to continue studies to develop these results.
Researchers now have the goal of conducting further studies to determine the possible impact of an earlier use of antibiotics on the microbiome of patients benefiting from a clinical trial. 39; observation subsequently funded by the biomedical research center of the NHRI on Biomedical Sciences. They add that future studies could examine whether rebalancing or increasing the microbiome could improve outcomes for patients.
These common antibiotics may increase the risk of colon cancer
David J. Pinato et al. Association of antibiotics predating the survival and response to immune checkpoint inhibitor therapy in cancer patients, JAMA Oncology (2019). DOI: 10.1001 / jamaoncol.2019.2785
Quote:
Antibiotics reduce survival rates for cancer patients treated with immunotherapy (September 13, 2019)
recovered on September 14, 2019
of https://medicalxpress.com/news/2019-09-antibiotics-survival-cancer-patients-immunotherapy.html
This document is subject to copyright. Apart from any fair use for study or private research purposes, no
part may be reproduced without written permission. Content is provided for information only.
[ad_2]
Source link