[ad_1]
In contrast, the United States has one of the weakest genomic surveillance programs of any rich country, Hanage said. “As it stands now, people like me are partnering with places and trying to beg them” for samples, he said on a recent call with reporters.
Other variant strains have been identified in South Africa and Brazil, and they share some mutations with the British variant. The fact that these changes evolved independently in multiple regions of the world suggests that they may present an evolutionary advantage for the virus. Yet another strain has recently been identified in Southern California; it was reported due to its growing presence in hard-hit cities like Los Angeles.
The southern California strain was detected because researchers at Cedars-Sinai, a hospital and research center in Los Angeles, have unrestricted access to patient samples. They could see that the strain has made up a growing share of hospital cases in recent weeks, as well as among the limited number of other samples taken at random from a network of laboratories in the region.
Not only does the United States do less genomic sequencing than most other wealthy countries, it also does its surveillance casually. This means that it takes longer to detect new strains and draw conclusions. It is not yet known, for example, whether the Southern California strain really deserved a press release.
Download the NBC News app for comprehensive coverage of the coronavirus outbreak
Large swathes of the privatized and decentralized U.S. health care system are not set up to send samples to public health or academic laboratories. “I’m more concerned with the variant detection systems than these particular variants,” said Nevada Public Health Laboratory director Mark Pandori, associate professor in the University of Nevada-Reno School of Medicine.
Limited genomic surveillance for viruses is yet another side effect of a fragmented and underfunded public health system that has struggled to test, track contacts and contain Covid-19 throughout the pandemic, Wroblewski said .
The country’s public health infrastructure, usually funded disease by disease, has decent systems for sequencing influenza, foodborne illness and tuberculosis, but there has been no national strategy for Covid-19. “To look for variations, it has to be a national image if it’s going to be done right,” Wroblewski said.
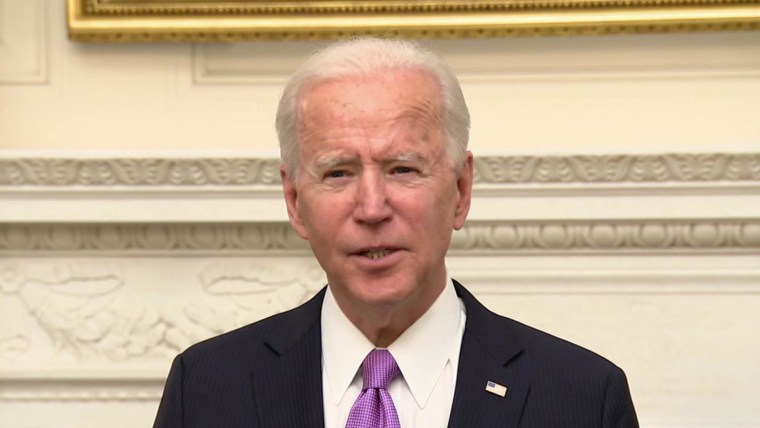
Last week, the Biden administration laid out a strategy for a nationwide response to Covid-19, which included expanded monitoring of variants.
So far, Covid-19 vaccines appear to protect against known variants. Moderna said his vaccine was effective against British and South African strains, although it produced fewer antibodies to them. The company is working to develop a revised dose of the vaccine that could be added to the current two-dose schedule as a precaution.
But a lot of damage can be done in the time it takes to roll out the current vaccine, let alone an update.
Even with limited sampling, the British variant has been detected in more than two dozen states, and the Centers for Disease Control and Prevention has warned that it could be the predominant strain in the United States by March. When it took off in the UK at the end of last year, it sparked an increase in the number of cases, overwhelmed hospitals and led to a holiday lockdown. Whether the United States faces the same fate could depend on the strains it competes against and the behavior of the public in the weeks to come.
Already risky interactions between people could, on average, become a bit riskier. Many researchers are calling for better masks and better indoor ventilation. But any update on the recommendations would likely play on the margins. Even if the variants spread more easily, the same recommendations that public health experts have been adopting for months – masking, physically distancing and limiting time spent indoors with others – will be the best way to stave off them, said Dr. Kirsten Bibbins-Domingo, physician. and professor at the University of California at San Francisco.
“The solutions are very sexy,” Bibbins-Domingo said. “But we need everyone to do them.”
This does not simplify the task. Masking remains controversial in many states, and the public’s patience to maintain physical distance has waned.
Adding to concerns: Even though case numbers have stabilized in many parts of the United States in recent weeks, they have stabilized at rates several times higher than they were in previous periods of the pandemic or in other parts of the world. Having all of this virus in so many bodies creates more opportunities for new mutations and new variants to emerge.
“If we keep letting this thing sneak up on it, it’s going to bypass any action we’re taking against it, and that’s the worst thing possible,” Pandori from Nevada said.
Compared to less virulent strains, a more contagious variant will likely require more people to be vaccinated before a community can see the benefits of widespread immunity. It’s a bleak prospect for a country that is already falling behind in the race to vaccinate enough people to bring the pandemic under control.
“When your best solution is to ask people to do things that they don’t like to do anyway, that’s very scary,” Bibbins-Domingo said.
KHN (Kaiser Health News) is a non-profit news service covering health issues. This is an editorially independent program of the KFF (Kaiser Family Foundation) which is not affiliated with Kaiser Permanente.
Follow NBC HEALTH on Twitter & Facebook.
[ad_2]
Source link