[ad_1]
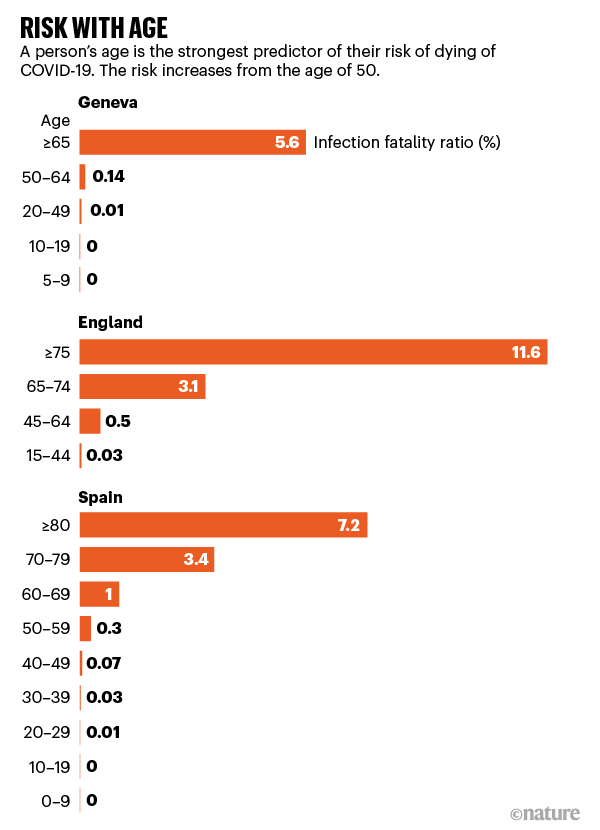
For every 1,000 people infected with the coronavirus who are under the age of 50, almost none will die. For people in their 50s and early 60s, about five will die – more men than women. The risk then climbs sharply over the years. For every 1,000 people infected in the mid-1970s or more, about 116 will die. These are the startling statistics obtained by some of the first detailed studies on the risk of death from COVID-19.
Trends in coronavirus deaths by age have been clear since the start of the pandemic. Research teams studying the presence of antibodies against SARS-CoV-2 in people in the general population – in Spain, England, Italy and Geneva, Switzerland – have now quantified this risk, says Marm Kilpatrick, researcher in infectious diseases at the University. of California, Santa Cruz.
“It gives us a much more precise tool when we ask ourselves what the impact might be on a certain population that has a certain demographics,” says Kilpatrick.
Studies show that age is by far the strongest predictor of an infected person’s risk of dying – a metric known as the Infection Mortality Ratio (IFR), which is the proportion of people infected with the infection. viruses, including those that have not been tested. or have symptoms, which will die of it.
“COVID-19 is not only dangerous for the elderly, it is extremely dangerous for people in their 50s, 60s and 60s,” says Andrew Levin, an economist at Dartmouth College in Hanover, New Hampshire, who has estimated that COVID -19 is more than 50 times more likely to be fatal for a 60-year-old than driving a car.
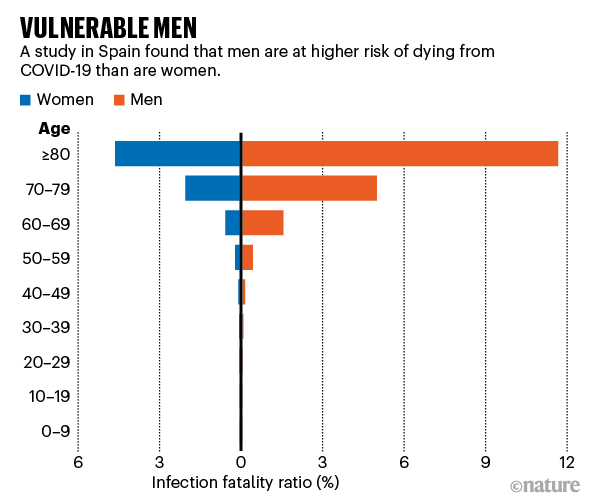
But “age can’t explain everything,” says Henrik Salje, an infectious disease epidemiologist at the University of Cambridge, UK. Gender is also a significant risk factor, with men almost twice as likely to die from the coronavirus as women. And the differences between countries in mortality estimates for older age groups suggest that the risk of dying from coronavirus is also related to underlying health conditions, the capacity of health care systems and the spread of the virus among people living in care facilities for the elderly. .
Older men are more at risk
To estimate the risk of age-specific mortality, the researchers used data from antibody prevalence studies.
In June and July, thousands of people across England received a pin-prick antibody test in the mail. Of the 109,000 randomly selected adolescents and adults who took the test, about 6% contained antibodies to SARS-CoV-2. This result was used to calculate an overall IFR for England of 0.9% – or 9 deaths in 1,000 cases. The IFR was close to zero for those aged 15 to 44, rising to 3.1% for those 65 to 74 and 11.6% for older people. The results of the study were published on the medRxiv preprint server1.
Another Spanish study which began in April and which tested antibodies in more than 61,000 residents of randomly selected households, observed a similar trend. The overall IFR for the population was around 0.8%, but it remained close to zero for those under 50, before rising rapidly to 11.6% for men 80 and over; it was 4.6% for women in this age group. The results also revealed that men are more likely to die from the infection than women – the gap widening with age.
“Men are twice as likely as women,” says Beatriz Pérez-Gómez, epidemiologist at the Carlos III Health Institute in Madrid, which participated in the Spanish study. The results were also published on the medRxiv server2.
Differences in the response of the male and female immune systems could explain the divergent risks, says Jessica Metcalf, a demographer at Princeton University, New Jersey. “The female immune system could have an advantage by detecting pathogens just a little earlier,” she says.
The immune system could also explain the much higher risk that older people die from the virus. As the body ages, it develops low levels of inflammation and COVID-19 could push the already overworked immune system overboard, says Metcalf. The worst outcomes for people with COVID-19 tend to be associated with an accelerated immune response, she says.
The study in England also compared the results of different ethnic groups. Mortality and morbidity statistics suggest that blacks and South Asians in England are more likely to die or be hospitalized. But the analysis, led by Helen Ward, an epidemiologist at Imperial College London, found that while blacks and South Asians were much more likely to have been infected than whites, they were no more likely to die from COVID-19.
Differences between countries
Researchers note that there is a marked difference in IFR estimates between some countries, especially for people aged 65 and over3. For example, an antibody prevalence study in Geneva estimated an IFR of 5.6% for people aged 65 and over.4. This was lower than estimates in Spain, which reaches around 7.2% for men and women aged 80 or older, and England, which found an IFR of 11.6% for those aged 75. or more.
There could be many explanations for these differences, says Andrew Azman, an infectious disease epidemiologist at the Johns Hopkins Bloomberg School of Public Health in Baltimore, Maryland, which was part of the Geneva study.
Countries with higher rates of comorbidities, such as diabetes, obesity, and heart disease, will have a higher IFR. However, countries whose health systems are better able to treat people severely affected by COVID-19 or whose hospitals were not overwhelmed during the height of the epidemic will have better survival rates, he says. .
Some of the differences could be attributed to how the different studies were conducted, the researchers say. For example, the differences in the reliability of antibody tests used in different studies, how COVID-19 deaths were recorded, and how researchers chose to divide populations by age.
There is some uncertainty in the data, so the estimates between studies may not be as different as they appear, says Lucy Okell, epidemiologist at Imperial College London, who participated in the English study.
But an important factor in the different death rates reported between countries appears to be the spread of the virus in nursing homes or elderly care facilities, says Salje.
In these places, people with fragile health live in tight-knit environments where the virus can spread quickly. When the UK study took care home deaths into account, the IFR among people aged 75 and over rose from 11.6% to 18.7%. Salje estimates that the IFR for Canada, where 85% of deaths occurred in nursing homes, would be significantly higher than that of Singapore, where nursing homes accounted for only 8% of deaths.
While death estimates are important in understanding the risk of spreading the virus to people of different age groups, they don’t tell the full story of the toll COVID-19 is taking, Kilpatrick says. “There is a fascination with death, but COVID-19 appears to cause a substantial amount of long-term illness,” he adds.
[ad_2]
Source link