[ad_1]
Reports indicate that there are now three vaccines for the coronavirus, with 90-95% effectiveness. What do reports do do not say, however, is: how will they be distributed? How can we get them? Or what will they cost? Or how long will they end the pandemic?
Correspondent David Pogue therefore decided to ask the experts: Now that you have the vaccine, what to do next?
“I have spent a career of over 35 years in vaccine development, and I cannot recall ever seeing a respiratory virus for which a vaccine provided such a high level of efficacy,” said Bill Gruber, head of vaccine development at Pfizer. . He supervised the testing of the Pfizer-BionTech vaccine on 44,000 volunteers.
His team learned the good news – that it was 95% effective – during a Zoom call. “They have tears in their eyes,” Gruber said. “It was an extraordinary, extraordinary moment.”
The new so-called RNA vaccines use a new approach. Instead of giving you a dead or weakened version of the virus itself (like the measles and chickenpox vaccines), these contain only a tiny fragment of the virus.
“It trains your immune system to fight off the virus when it encounters it in the future,” Gruber said. “This is a watershed moment in two ways: because it’s obviously safe and effective for the coronavirus, but it could also really be a pivotal moment in the ability to develop better vaccines.”
Pfizer has tested several different formulas for the vaccine (or constructs, as they call them).
“We didn’t know which one would work the best,” Gruber said. “We moved very methodically, but quickly.”
But vaccine development is only the first hurdle. Now you need to send it to people.
Thomas Tighe, CEO of Direct Relief, a non-profit organization that distributes drugs to community health centers and free clinics, explained, “It ranges from manufacturers and distributors to CVS and Walgreens and RiteAids around the world, directly to doctors’ offices. ”
And you gotta keep it cold. Some vaccines drop to -70 degrees Celsius [-94 Fahrenheit]. Ultra-cold!
Tighe introduced Pogue to the concept of the cold chain for drug distribution.
“If you buy ice cream, you get food through a cold chain. It’s made, it’s kept cold until it gets to your grocery store’s distribution center, where you’re the picker. and the conditioner. You are your last mile. ”
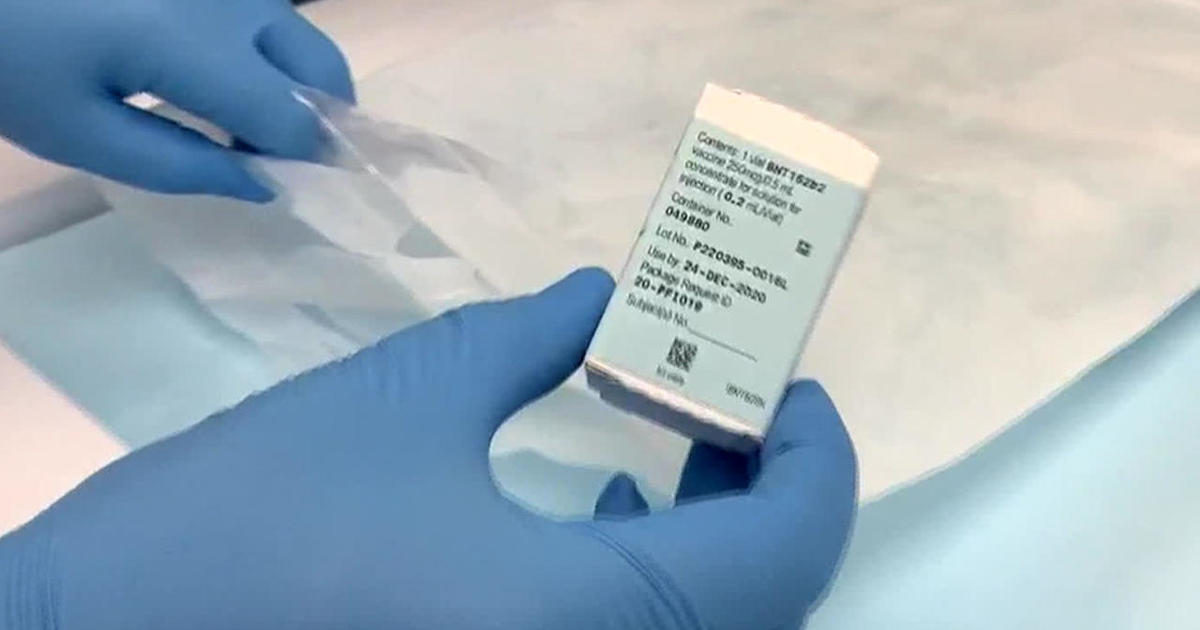
If the FDA gives approval to the new coronavirus vaccines, some of them will soon be crossing the country in special containers surrounded by super-frozen plates. They assemble the tiles around the box, enveloping it in cold. The temperatures of each box can be monitored throughout its journey via GPS.
CBS News
And for use in airplanes and trucks, there’s a battery-powered, self-contained shipping freezer. “On a forklift you can bring this,” Tighe said. “It is rated at -20 Celsius, -4 Fahrenheit.”
“It appears there is a big difference between the Pfizer vaccine with its -94 requirements and Moderna, which could survive in many of these existing cold technologies,” Pogue said.
“The temperature difference is significant,” Tighe said.
The next challenge is to make enough vaccine. Pfizer, Moderna, and the other drug companies are already making their vaccines in huge tanks, 24 hours a day. In fact, they started months ago, even before the trials were completed.
“They have to come up with 330 million doses?” Pogue asked.
“Oh, no, no, it’s much more than that,” said Willy Shih, Harvard Business School professor, economist and manufacturing expert. “We should think ten times as much, at least, as a starting point. We should think about three and a half billion doses.”
And shipping companies are already preparing: “Many carriers, like FedEx, like UPS, like DHL, have built these freezer farms in anticipation of having to ship larger quantities of COVID-19 vaccines in very cold temperatures,” Shih says .
The biggest problem, Shih said, will be managing our expectations. The pandemic won’t end once you get your vaccine: “I’m really worried about this, people don’t understand -” I had this vaccine, I should be good, right? I can go back to dinner. I can have my hair cut You know I can go to the gym. Not so fast. Certainly, until we get wider immunization, people will still have to wear masks and they will still have to practice social distancing.
“I don’t think the American public is ready for this yet,” he said.
“I was probably, along with much of the country, thinking, ‘This is the beginning of the end of the pandemic,'” Pogue asked.
“No,” Shih replied. “It is only when the contagion rate decreases that we will return to some semblance of normalcy.” And it will take time.
The government plans to allocate vaccines to states based on their populations. The vaccine will be free for everyone. The CDC will recommend giving it to healthcare workers and older Americans first. If all goes well, by spring 2021 the vaccine will be available to anyone who wants it.
But the question is: will enough people want it?
“Convincing people to get vaccinated is going to be our biggest challenge of all,” said Céline Gounder, epidemiologist at NYU Grossman School of Medicine and Bellevue Hospital. “In the United States, we have a history of vaccine skepticism.
There are people who do not want the government to say what to do. You have people who don’t trust pharmaceutical companies. You also have communities of color that have long been suspicious of the health care system. “
Pogue asked, “It might sound like a really stupid question, but what are people worried about?”
“People are afraid of side effects,” Gounder replied. “They’re afraid of getting sick. I’ve even heard theories that people think it’s a vaccine for mind control. Much of it is all over the map. We have a way. really hard to do to convince people. It isn’t. “
“So you are a member of President-elect Biden’s Advisory Committee on Coronavirus; Is there a plan in place to address some of the skepticism? ”
“We’re going to have to think outside the box here and be a little creative,” Gounder replied. “It’s something we haven’t had to do here before.”
“Are you considering public service announcements and celebrity referrals?” Pogue asked.
“It doesn’t really think outside the box,” she said. “I think you’re going to have to see a lot more grassroots community outreach, in partnership with local leaders, people the community trusts.”
Pogue said, “Well, let me ask you this, Dr Celine Gounder, on national television: would you take the Pfizer or Moderna vaccine for you and your family now?”
“I’ll probably be one of the first in line to get it,” she replied. “I am a frontline health worker. So, I would really like to get the vaccine before I have to put myself in danger again this way. “
“Aren’t you worried about mind control?”
“I’m not worried about mind control!” Gounder laughs.
The reputation of the AstraZeneca vaccine has suffered as a result of reporting test irregularities. But as for the Pfizer and Modern vaccines, the whole story seems unlikely; the stakes were high, the company was shut down, and somehow researchers and scientists came up with a new type of vaccine that they said was 95% effective – within months .
Pogue asked Pfizer’s Bill Gruber how this was even possible.
“We are living in remarkable times,” he said. “Science has really advanced to the point where we have the tools to do this kind of thing. And we have dedicated people to do it, people who have dedicated their lives. You know, everyone rowers together, and that’s a really amazing thing. It wouldn’t have happened without it. “
For more information:
Story produced by Gabriel Falcon. Publisher: Ed Givnish.
[ad_2]
Source link
