[ad_1]
We still struggle to understand whether infection with SARS-CoV-2, with or without COVID-19 symptoms, offers protection against other infections. Antibodies are an indicator of immunity and are the easiest part of the immune response to follow. But the data indicates that antibody generation is highly variable, and their production can start to wane within months. But there are many other aspects to the immune response, many of which are T-cell centered. And again, the response seems extremely complex.
Now, more studies are being published on other specialized aspects of the immune response. While these results provide some reason for optimism in terms of lasting immunity, there are still a large number of unknowns.
Go with the flow
The two studies we are going to look at were made possible by a technique called “flow cytometry” which has been shown to be very useful in studying the immune response. Essentially, it helps researchers overcome the biggest problem in these studies: There is an abundance of very similar cells involved in an immune response. While a trained eye can distinguish a T cell from a macrophage using a microscope, knowing that there are T cells doesn’t tell us much. Not only would we like to know how many there are, but we would need to know what types of T cells are present. T cells can help in the production of antibodies, they can kill infected cells, they can be used to remember exposure to pathogens, etc.
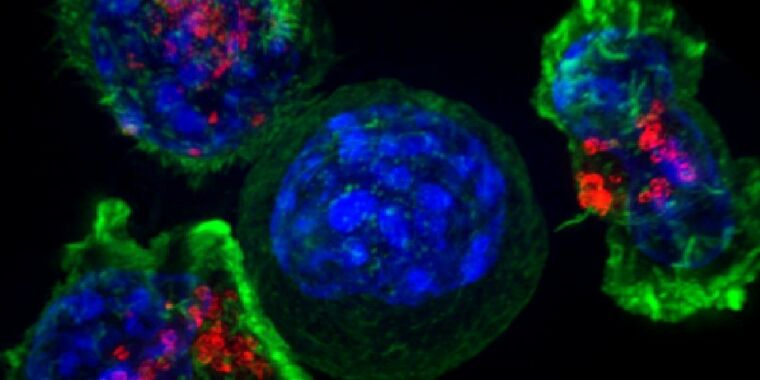
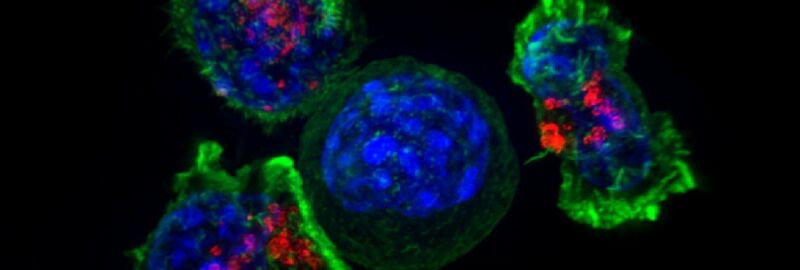
Flow cytometry can help us find out which cells are actually present. This involves taking immune cells from a blood sample and passing them one by one through the sensors. Each of these sensors can examine an aspect of the cell. Typically, you label cells with a fluorescent molecule that only sticks to specific cell types and use a laser to determine if the molecule is present as the cell flows. After the sensor, the device can redirect the flow to separate cells with and without these molecules.
So if you make a fluorescent molecule that will stick to T cells, you can figure out how many T cells are there and pull them all apart. The bottom line is that it can be done iteratively. Once you have the T cells, you can add another tag and separate a single population of T cells, like killer T cells. And then you can separate the specific types of killer T cells from that population. Meanwhile, the other population – anything that isn’t a killer T cell – can also be sorted, allowing researchers to extract memory T cells, and so on.
This can give us an idea of the cells present when an infection is in progress. But not just that, its final output is a pure population of specialized cells, which can then be examined in more detail to try and figure out what they do.
Obviously, the more tags you can use to separate cells, the more detailed your analysis can be. And, in this case, the researchers had access to equipment that could do a lot of separation: almost 30 individual beacons were used to separate different populations of cells. (Both articles have researchers at the Karolinska Institute in Sweden, where this sophisticated machinery is likely to reside.)
I remember this
In a paper, the research team focused on finding the types of T cells present in people with SARS-CoV-2, as well as what happens after the virus is cleared. Overall, the researchers had samples from over 200 people and data on their clinical outcomes – they knew which people had severe cases and could potentially correlate that with the presence of specific types of immune cells.
It turned out that those with active infections produced a lot of killer T cells, which target infected cells and kill them. The research team also found a difference after the infection had run its course. Here, people with symptoms, mild or severe, appear to have produced more memory T cells, ready to fight off another SARS-CoV-2 infection.
The presence of these memory T cells was unrelated to whether the individual was producing antibodies against the virus, suggesting that they could serve as an alternative route for immune protection. Emphasis on “power”. The researchers stress that “it remains to be determined whether robust responses of memory T cells in the absence of detectable circulating antibodies can protect against severe forms of COVID-19.” The shelf life of these memory cells also remains in the “unknown” category – the answer is “over a decade” for SARS and MERS.
As in other recent studies, these researchers found that there were T cells on the verge of responding to SARS-CoV-2 even in people who had never been exposed to it, possibly due to exposure to coronaviruses that cause cold-like symptoms. Again, whether this provides any protection is not at all clear.
No more killers
T cells are not the only ones that can kill infected cells; there is another type of blood cell called a natural killer that does this as well. While T cells are adaptive – they recognize a specific characteristic of a pathogen due to a unique receptor structure – natural killers largely recognize cells infected with entire classes of pathogens. So, using the same flow cytometry equipment that was used in the other article, another research team analyzed what was happening with natural killers in a small population of patients with COVID-19 (mild cases and serious).
As one would expect, the natural killer cells had indications that they were activated by infection with SARS-CoV-2, producing immune signaling molecules and dividing to make more of these cells. But there was little difference in this regard between those with mild and severe symptoms. There were, however, other differences which apparently correlated with the severity of the disease. More specifically, these include the production of the protein used to kill infected cells, which is much more common in samples taken from patients with severe cases. The cells of those with severe cases have also shown more evidence to be involved in an inflammatory response.
In contrast, natural killer cells from people with mild symptoms of COVID-19 tended to have high levels of what is called a “checkpoint” protein. These proteins help stop cell activity unless certain conditions are met, and therefore could be involved in attenuating the response of natural killers.
Cause and effect
The challenge here, unfortunately, is to separate cause and effect. It is not clear whether a more aggressive response from natural killer cells produces the problems that arise from an excessive inflammatory response and thus contributes to the severity of the disease; it could simply be that more serious illness is leading to a more aggressive natural killer response.
Taken together, these two articles – and many more that continue to be published weekly – provide an increasingly detailed examination of the activity of the immune system in response to SARS-CoV-2. Unfortunately, the image they paint is extremely complex and does not fit neatly into a simple image that might help with politics or treatments. T cells clearly retain a memory of exposure to SARS-CoV-2, but it is not clear whether this is protective in the long term. Certain types of immune cells are more active in severe cases, but it is not clear if we can identify this well in advance to tailor treatments.
Over time, a clearer picture will gradually emerge from the cumulative evidence that each of these studies provides. But it will take time and the likelihood of a single study providing a clear picture or a breakthrough is low.
Cell, 2020. DOI: 10.1016 / j.cell.2020.08.017;
Science Immunology, 2020. DOI: 10.1126 / sciimmunol.abd6832 (About DOIs).
[ad_2]
Source link