[ad_1]
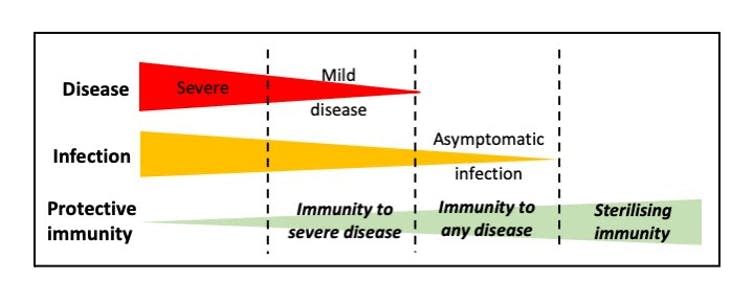
Vaccines are a wonder of medicine. Few interventions can claim to have saved so many lives. But you might be surprised to know that not all vaccines provide the same level of protection. Some vaccines prevent you from getting symptomatic illness, but others also prevent you from getting infected. The latter is called “sterilizing immunity”. With sterilizing immunity, the virus cannot even implant itself in the body because the immune system prevents the virus from entering cells and replicating itself.
There is a subtle but important difference between preventing disease and preventing infection. A vaccine that “just” prevents disease may not stop you from passing the disease to others – even if you are feeling fine. But a vaccine that provides sterilizing immunity stops the virus in its tracks.
In an ideal world, all vaccines would induce sterilizing immunity. In fact, it is actually extremely difficult to produce vaccines that completely stop the viral infection. Most of the vaccines in common use today do not achieve this goal. For example, vaccines targeting rotavirus, a common cause of diarrhea in infants, are only able to prevent serious illness. But it has always proven invaluable in controlling the virus. In the United States, there have been nearly 90% fewer cases of hospital visits associated with rotavirus since the vaccine was introduced in 2006. A similar situation occurs with current polio vaccines, but it is hoped that this virus can be eradicated on a global scale.
The first SARS-CoV-2 vaccines to be licensed have proven to be very effective in reducing the disease. Despite this, we do not yet know whether these vaccines can induce sterilizing immunity. It is expected that data addressing this issue will soon be available from ongoing vaccine clinical trials. Even if sterilizing immunity is induced initially, this can change over time as immune responses decline and viral progression occurs.
Immunity in individuals
What would a lack of sterilizing immunity mean for people vaccinated with the new COVID vaccines? It just means that if you come across the virus after vaccination, you can get infected but have no symptoms. This is because your vaccine-induced immune response fails to prevent each viral particle from replicating.
It is generally understood that a particular type of antibody called a “neutralizing antibody” is needed to sterilize immunity. These antibodies block the entry of the virus into cells and prevent replication. However, the infecting virus may need to be the same as the vaccine virus in order to induce the perfect antibody.
Fortunately, our immune responses to vaccines involve many different cells and components of the immune system. Even if the antibody response is not optimal, other aspects of immune memory can intervene when the virus invades. These include cytotoxic T cells and non-neutralizing antibodies. Viral replication will be slowed down and therefore the disease will decrease.
We know this from years of study of influenza vaccines. These vaccines generally induce protection against disease, but not necessarily protection against infection. Much of this is due to the different strains of influenza circulating – a situation that can also occur with SARS-CoV-2. It is reassuring that influenza vaccines, although they cannot induce sterilizing immunity, are still extremely useful in controlling the virus.

Immunity in a population
In the absence of sterilizing immunity, what effect might SARS-CoV-2 vaccines have on the spread of a virus in a population? While asymptomatic infections are possible after vaccination, there are fears that SARS-CoV-2 may continue to infect as many people as before. Is it possible?
People who are asymptomatically infected usually produce viruses at lower levels. While there is no perfect relationship, usually more virus equals more disease. Therefore, vaccinated people are less likely to transmit enough virus to cause serious illness. This in turn means that those infected in this situation will transmit less virus to the next susceptible person. This has been clearly demonstrated experimentally using a vaccine targeting a different virus in chickens; when only part of a flock was vaccinated, unvaccinated birds still had milder disease and produced less virus.
Thus, while sterilization of immunity is often the ultimate goal of vaccine design, it is rarely achieved. Fortunately, this hasn’t stopped many different vaccines from drastically reducing the number of cases of viral infections in the past. By reducing levels of disease in individuals, it also reduces the spread of the virus in populations, which will hopefully bring the current pandemic under control.
This article is republished from The Conversation under a Creative Commons license. Read the original article.

Sarah L Caddy does not work, consult, own stock, or receive funding from any company or organization that would benefit from this article, and has not disclosed any relevant affiliation beyond her academic appointment.
[ad_2]
Source link