
[ad_1]
Sign up here for our daily coronavirus newsletter on what you need to know, and Subscribe to our Covid-19 podcast for the latest news and analysis.
The United States has spent months trying to vaccinate those most at risk of serious illness against Covid-19, from healthcare providers to the elderly, essential workers and those with other conditions. underlying health issues.
In the coming weeks, data on hospitalizations and deaths at Covid will show whether this strategy is working.
Spikes in the number of cases usually translated weeks later into increased hospitalizations and deaths, a dynamic that is expected to weaken after the most vulnerable are vaccinated. While there are early signs occurring in places like nursing homes, it remains to be seen whether this will be true for other at-risk groups and young people. And the moment of truth comes just like the infections again in many states.
“This will be a test of the effectiveness of our vaccination campaigns in reaching populations at risk,” said Josh Michaud, associate director of global health policy at the Kaiser Family Foundation, an independent non-profit organization. All states have at least made people aged 65 and over eligible, which means “you’re removing something like 80% of the population most at risk of dying”.
The growing share of Americans who have received Covid-19 vaccines – about 26%, or more than 87 million people, have at least one dose – represents an inflection point in the pandemic’s trajectory and a watershed moment for the United States, where the virus has sickened at least 30 million and killed more than 547,000.
Yet most people in the United States are still unprotected. And there are major hurdles in America’s race to stay ahead of the virus, including vaccine reluctance and barriers to access, declining testing and the emergence of more contagious variants. .
While the number of new cases, hospitalizations and deaths will remain important indicators of the state of the pandemic, there is a dire need for more accurate ways to measure Covid-19, according to public health experts.
“Knowing where we have a problem by community and by source is very important in managing the pandemic as we move forward,” said Ali Mokdad, professor at the Institute for Health Metrics and Evaluation in Seattle, which produces influential Covid-19 projections. “Otherwise, we are flying blind.”
Shift Younger
At least for some groups, Covid vaccines are reaching their target audience and doing what they’re supposed to do. Among people aged 65 and older, an early demographic to qualify for inoculation, about 71% received at least one dose, according to the Centers for Disease Control and Prevention. The data.
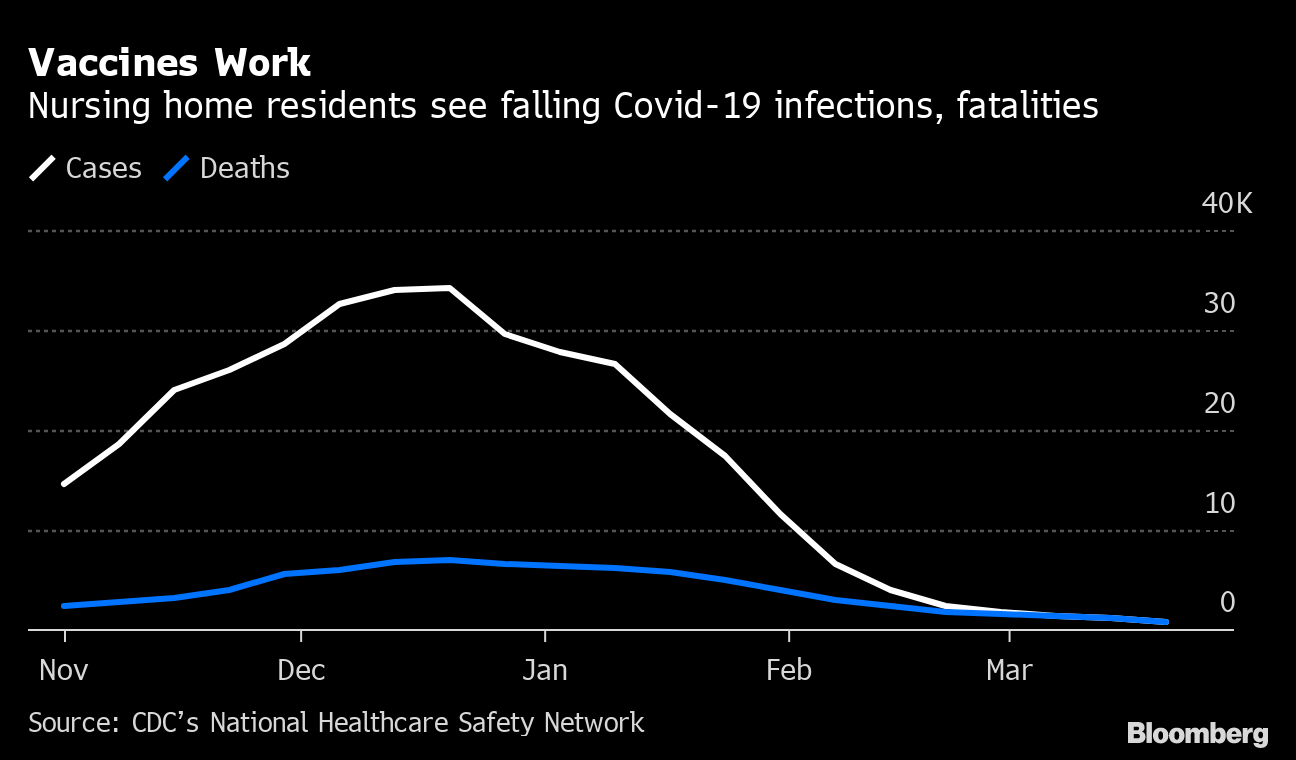
In nursing homes, where residents were also prioritized early for vaccines, Covid cases among residents have fallen by nearly 98% since mid-December and deaths by 88%, according to the CDC. data, which industry officials have linked to vaccinations.
This means that new cases of Covid will likely emerge in younger age groups. This happened in Israel, where infections recently plateaued despite the country’s leading vaccination program. It turned out that cases among young people were increasing, even as infections were decreasing in those 50 and over.
Younger people, even though they are thought to be less likely to show symptoms, can still spread the virus and contract severe cases on their own. In a handful of states, for example, people with underlying health conditions are not yet eligible for vaccines.
Vaccines work
Nursing home residents see drop in Covid-19 infections, deaths
Source: CDC National Healthcare Safety Network
While it is “very good news that our death rate is decreasing among those who have been vaccinated, there is still a death rate among those over the age of 20,” CDC director Rochelle Walensky said at the meeting. ‘a White House briefing this week. “As these cases continue to increase in this demographic group, we will also see death rates in this demographic group.”
Those risks are a priority in West Virginia, which expanded eligibility this week in a bid to interrupt transmission of the virus among young people.
“We think this will save us more time,” said Clay Marsh, West Virginia Covid-19 coordinator and executive dean for health sciences at the University of West Virginia. “We would love to keep the variants at bay and try to get a large chunk of the rest of the population vaccinated.”
In Michigan, where Covid infections are on the rise again, the hospitalization-to-case ratio is significantly lower than it was in October, the last time the state saw an increase of this magnitude. About 69% of its 65-and-over cohort – which typically accounted for half of all Covid hospitalizations and around 4 in 5 deaths – have now received at least one dose of a vaccine.
Yet the The Michigan Health & Hospital Association sounded the alarm this week about the peak in hospitalizations among younger age groups: since early March, they have increased 633% among 30-year-olds and 800% among those in their 40s. . The data shows that Covid-19 vaccines work but also “that adults of all ages are vulnerable to complications from the disease,” the group said.
Blunt instrument
While expanding immunization coverage is key to recovery in the United States, it also threatens to further shatter an already fractured national response to the pandemic.
Take, for example, test levels, which identify and count cases in the United States. In recent months, these levels have stagnated and have even recently started to decline.
“We have completely shifted our focus to vaccines at the expense of testing,” with states even converting testing facilities to administer injections, said Jennifer Nuzzo, senior researcher at the Johns Hopkins Center for Health Security, adding that “we are potentially losing insight into where the virus is, where it is not, and how quickly it is spreading. “
And while there are other ways to monitor Covid trends known as surveillance, such as performing more targeted testing in places like travel centers, nursing homes, or prisons, which don’t ‘have never started in the United States, Nuzzo said.
This is important because as vaccine coverage grows, viral epidemics are likely to become more dispersed.
“People would be surprised how many people still go unvaccinated, especially among vulnerable groups,” said David Rubin, physician and director of PolicyLab at Children’s Hospital of Philadelphia, which modeled the spread. of Covid-19.
CDC epidemiologist Adam MacNeil said in an interview that the agency is setting up surveillance systems to track re-infections of Covid-19 and cases in which people who have been vaccinated are infected , to support long-standing efforts to track and model infection levels.
Federal and state authorities have made county-level virus data public, but more precise analyzes of those affected are often lacking, IHME’s Mokdad and others said. Data on cases and hospitalizations by age group and race or ethnicity, for example, is rarely and inconsistently available at the county level, according to PolicyLab’s Rubin.
“We don’t even have that, a year after the start of the pandemic,” he said.
– With the help of Jonathan Levin and Jill R Shah
[ad_2]
Source link