[ad_1]
09 July 2018
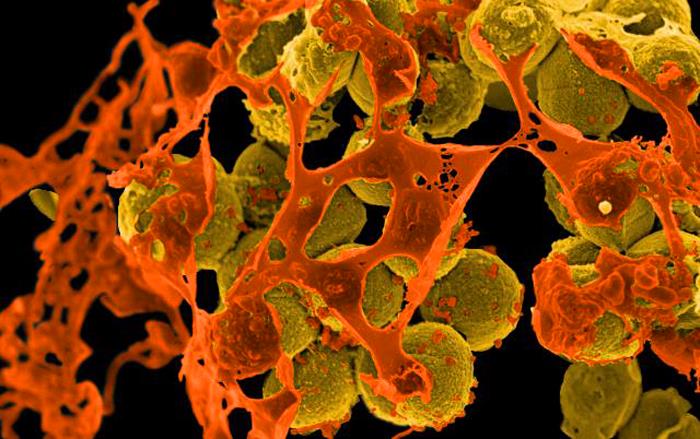
The early release of a second anti-MRSA antibiotic against vancomycin could reduce mortality in severe cases of pediatric co-infection with MRSA virus. Photo credit: NIAID
According to data published in Clinical Infectious Diseases the early addition of a second antibiotic resistant to methicillin Staphylococcus aureus (MRSA) with vancomycin can reduce mortality in severe cases of MRSA co-infection in children.
Co-infection with influenza and MRSA can cause life-threatening necrotizing pneumonia in children and is badociated with high rates of death in critically ill children. Investigators prospectively included 170 children under 18 years old with influenza infection and acute respiratory failure in 34 pediatric intensive care units from November 2008 to May 2016.
L & # 39; Study compared 3 conditions: co-infection with MRSA, non-MRSA bacterial co-infection, and no bacterial co-infection – in terms of clinical course, therapy, and baseline characteristics.
Co-infection with influenza and MRSA was more frequently badociated with leukopenia, acute lung injury, use of vasopressors, maintenance of cardiopulmonary bypbad and mortality compared with both non-influenza groups. -SARM. Influenza-related mortality was 40% with MRSA and only 4.3% without (relative risk [RR] 9.3, 95% CI, 3.8-22.9).
Mortality in children with MRSA receiving vancomycin within 24 hours after hospitalization (n = 29/30) dropped to 12.5% (n = 2/16) when treatment included a second anti-MRSA antibiotic within 24 hours. % (n = 9/13) with vancomycin monotherapy (RR, 5.5, 95% CI 1.4, 21.3 P = 003).
Children with severe comorbid conditions who predisposed them to influenza were excluded from the study, decreasing potential confounders, but also generalizability. The design of the study was observational and the fact that the cohort of MRSA patients was relatively small further limited the results. The researchers also noted that because co-infection with MRSA can occur with other viruses and that the study focuses only on the flu, it is impossible to determine if the clinical course and the results of co-infection with MRSA are similar.
The study provides "real evidence" of the effectiveness of antibiotics in co-infections with infant-MRSA flu. The researchers also suggested that "a continuous national registry of these life-threatening co-infections in children, with antibiotic susceptibility testing, antibiotic management, and clinical specimen collection, could help guide care."
Reference
Randolph A, Xu R, Novak T, et al. Vancomycin monotherapy may be insufficient to treat methicillin-resistant staphylococcus aureus co-infection in children with severe influenza-related illness [published online June 9 2018]. Clin Infect Dis . doi: 10.1093 / cid / ciy495
[ad_2]
Source link