[ad_1]
Then, the Moderna vaccine became available to health professionals in the city. She received her first injection of Covid-19 about a week before her scheduled mammogram.
Quasha didn’t notice much reaction to the vaccine at first, but a few days before her appointment, her left arm started to hurt.
Tender, swollen bumps developed under his left armpit, along with a large swelling above his collarbone – all areas where the body has lymph nodes, the body’s filters for germs.
“You have lymph nodes above and below your collarbone,” Quasha said. “You don’t want to feel that way. It was scary when I felt it.”
Lymph nodes contain immune cells that help fight invaders. That is why it made sense to Quasha that the nodes reacted to the vaccine, building antibodies as they were designed to do. But she couldn’t be sure.
The swelling was only on the left side where she had had the blow – the same side as the disturbing bump. Was it a reaction to the vaccine or some other sign of breast cancer?
‘It was like a forest fire’
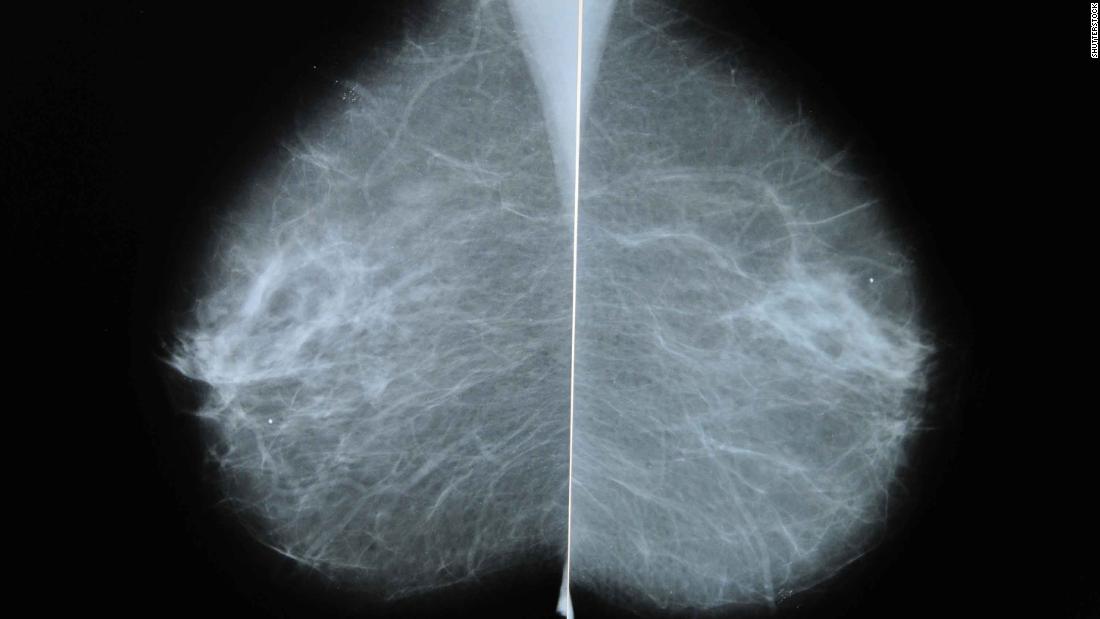
After the ultrasound, Quasha’s radiologist was worried. She told Quasha that she considered the lump she felt in her chest to be Of little importance, but the lymph nodes that showed up as white spots on her mammogram were another matter.
In a non-pandemic period, this finding would set off alarm bells, requiring the need for further investigation, even an immediate biopsy. However, Quasha had just been vaccinated. After discussing it with her, Quasha said her doctor decided not to do a biopsy at this time. Instead, she told Quasha to come back for a follow-up ultrasound in six weeks.
Similar scenarios have occurred in mammography centers across the country. As radiologists compared their notes to colleagues, the word started to spread.
“We all started talking about it, and it was like a wildfire,” said Dr. Connie Lehman, head of breast imaging in the Massachusetts General Department of Radiology.
“I can’t tell you how many women get knots on mammograms and people thought it wouldn’t be that common,” said Lehman, who is also a professor of radiology at Harvard Medical School.
“We wanted to make the point that women don’t always need to have a biopsy,” said Dr Lars Grimm, associate professor of radiology at Duke University School of Medicine and one of the authors of the SBI opinion. “Because often the default if you see swollen lymph nodes in a patient would actually be to recommend a biopsy.”
Lehman of the Mass General agreed. “When you hear hoof beating, don’t think of the zebra,” she says. “If a woman had a vaccine in her arm on the same side, and the lymph nodes are swollen, that’s a normal biological response. It’s totally expected. It just doesn’t make sense to start imaging. . “
This does not mean that women who wish to be sure of their cancer status cannot have a biopsy, Grimm pointed out.
“You actually have women who want to do a biopsy,” he says. “You could say to them, ‘Hey, I think it’s due to your Covid vaccine, and I’m sure it’ll go away in a few weeks on its own and you’ll be fine.’ But this patient tells you, “I won’t be comfortable waiting, I want to know now. “
Focus on screening to save lives
For Quasha, knowing that many women had the same type of reaction to the vaccine was a welcome relief from the worry. After a discussion with her doctor, she said she no longer needed the follow-up screening.
“I was very reassured,” Quasha said. “The point here is that there are a number of side effects of the vaccine which are not dangerous but can sometimes increase patient anxiety.”
Instead of bringing women back for an unnecessary ultrasound, radiology centers should focus on scheduling women who have missed or are late for their mammograms, Lehman said.
“We need to take care of the large percentage of women who have not been screened due to closures during Covid,” she said. “In Mass General alone, we have failed to screen 15,000 women due to Covid, and we are still trying to bring them back.
“This is not where I have to start doing axillary ultrasounds, because someone has had a vaccine and the knot has swollen. It is just not practical or pragmatic or does not meet our needs. patient first, ”she said.
It’s not just breast cancer, Lehman pointed out. Lymph nodes in other parts of the body also respond to Covid-19 vaccines, forcing people with other forms of cancer to undergo unnecessary procedures.
“There were a few false alarms and unnecessary biopsies because people didn’t remember to ask, and they’re assuming the knot was recurring cancer,” she said.
What to do?
To avoid unnecessary worry, SBI recommends that women schedule routine annual breast screening before receiving the Covid-19 vaccine. If a woman has already received the vaccine, or is due to do so soon, the company suggests waiting at least four to six weeks after the second dose before making an appointment.
At Mass General, Lehman and his team went further. They screen all women, regardless of their vaccine status, but tell those without a history of cancer that any lymph node swelling that could be linked to a Covid-19 vaccine is benign – c that is, non-cancerous.
“If their concern is swelling or tenderness after the vaccine in their armpits, we suggest they wait four to six weeks, talk to their doctor, and if it persists, we bring them in for an evaluation. “, she said.
Whatever you do, experts point out, don’t skip breast cancer screening when recommended. A study published Tuesday in the journal Radiology that followed more than half a million women made the point clear: Women who skip even a scheduled mammogram screening before being diagnosed with breast cancer have a significantly higher risk of dying.
In fact, the risk of getting fatal breast cancer within 10 years of diagnosis was 50% lower for women who had regular breast screenings, according to the study.
[ad_2]
Source link