[ad_1]
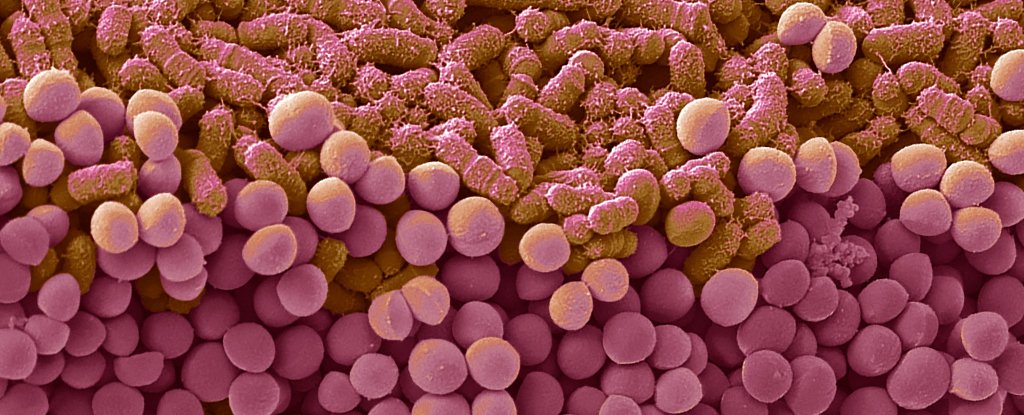
Our guts are fabulous places, filled with a myriad of germs. These tiny life forms help us with everything from fermenting fiber to feeling full. But their effects don’t just stay in the gut.
We know that gut microbes like bacteria and yeast have a role to play in diabetes, depression, and neurovascular disease. Today, scientists have discovered that molecules produced by bacteria in the stomach can give the human body a helping hand with the immune system, even going so far as to help fight tumors.
“The results are an example of how the metabolites of intestinal bacteria can modify the metabolism and gene regulation of our cells and thus positively influence the effectiveness of tumor therapies,” explains immunologist Maik Luu of the University Hospital of Würzburg in Germany.
Short-chain fatty acids (SCFAs) are one of the useful molecules produced when dietary fiber is fermented in the gut. The main SCFAs are acetate and butyrate, as well as the less common pentanoate, which is only found in certain bacteria. All of these SCFAs have many positive effects on human health, such as regulating insulin resistance, cholesterol, and even appetite.
Luu and his colleagues have now found that butyrate and pentanoate also stimulate the anti-tumor activity of a type of killer T cell known as CD8, by reprogramming how they work. For the first time, they have demonstrated it experimentally in mice.
“When short-chain fatty acids reprogram CD8 T cells, one of the results is an increase in the production of pro-inflammatory and cytotoxic molecules,” says Luu.
“We were able to show that short chain fatty acid butyrate and, in particular, pentanoate are able to increase the cytotoxic activity of CD8 T cells.”
Using lab mice, the team discovered that certain commensal bacteria produce pentanoate. For example, a relatively rare human intestinal bacteria, Megasphaera Marseille small improved proteins called cytokines in killer T cells, leading to an increased ability to destroy tumor cells.
As a control, the team experimented with other non-pentanoate-producing bacteria and found no effect on cytokine levels. This finding could be particularly useful for therapies that harness the immune system to fight cancer.
Some tumor cells have proteins on their surface that can bind to T cell proteins, resulting in a “checkpoint” immune response that tells the killer cell to spare its target – in this case, the cancer cell. . Immune checkpoint inhibitor (ICI) therapy works by blocking these checkpoint proteins, allowing T cells to do their job and destroy tumor cells.
“A defined commensal consortium of 11 human bacterial strains elicited strong anti-tumor immunity mediated by CD8 + T cells,” the team writes in their new paper.
“This study demonstrated that a mixture of scarce human commensals was able to dramatically improve the efficacy of ICI therapy in mice.”
This exciting discovery brings us closer to understanding how the right mix of gut bacteria could help boost ICI therapies given to cancer patients.
The team also looked at a type of genetically engineered T cells called CAR-T cells that are used in immunotherapy, and found that bacterial assist works the same way, especially in solid tumors.
While researchers warn there’s a long way to go before these results can be applied in the clinic, this important finding is another reason to love your gut bacteria and remember to eat more fiber.
The research was published in Nature Communication.
[ad_2]
Source link