[ad_1]
Blood tests are no fun.
They hurt. The veins may burst, or even roll – as if they are also trying to avoid the needle.
Often, doctors use blood samples to look for biomarkers of the disease: antibodies that signal a viral or bacterial infection, such as SARS-CoV-2, the virus that causes COVID-19, or cytokines indicating inflammation observed in conditions such as rheumatoid arthritis and sepsis.
These biomarkers aren’t just in the blood, however. They are also found in the dense liquid medium that surrounds our cells, but in low abundance which makes them difficult to detect.
Until now.

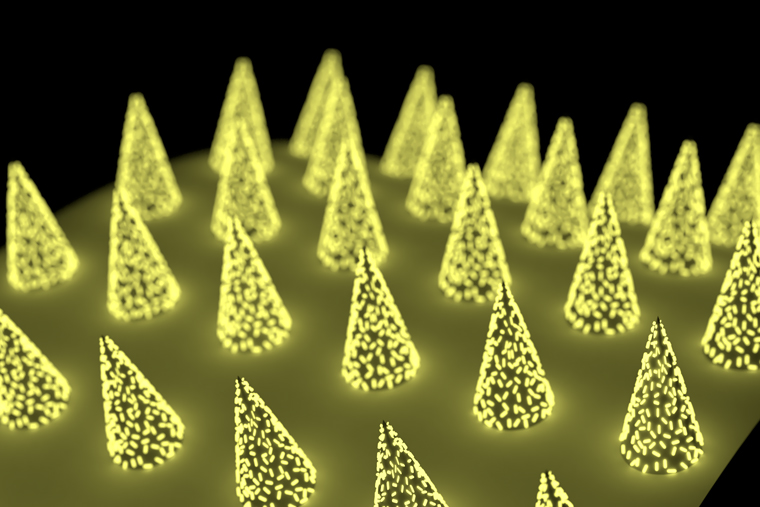
Engineers at the McKelvey School of Engineering at the University of Washington in St. Louis have developed a micro-needle patch that can be applied to the skin, capture a biomarker of interest and, thanks to its unprecedented sensitivity, allow clinicians to detect its presence.
The technology is inexpensive, easy to use for clinicians or patients themselves, and could eliminate the need to go to the hospital just for a blood test.
The research, from the lab of Srikanth Singamaneni, Professor Lilyan & E. Lisle Hughes in the Department of Mechanical Engineering and Materials Sciences, was published online Jan. 22 in the journal Nature Biomedical Engineering.
In addition to the low cost and ease of use, these microneedle patches have another advantage over blood tests, perhaps the most important feature for some: “They are almost painless,” said Singamaneni.
Finding a biomarker using these micro-needle patches is similar to a blood test. But instead of using a solution to find and quantify the biomarker in the blood, the microneedles pick it up directly from the fluid that surrounds our cells in the skin, called dermal interstitial fluid (ISF). Once biomarkers have been captured, they are detected in the same way – using fluorescence to indicate their presence and quantity.
ISF is a rich source of biomolecules, densely packed with everything from neurotransmitters to cellular waste. However, to analyze biomarkers in ISF, the conventional method generally requires extraction of ISF from the skin. This method is difficult and generally the amount of ISF that can be obtained is not sufficient for analysis. This has been a major obstacle for the development of bio-sensing technology based on microneedles.
Another method involves the direct capture of the biomarker in ISF without having to extract the ISF. Much like attending a crowded concert and trying to make its way to the front, the biomarker has to maneuver through a vibrant, crowded EWB soup before reaching the micro-needle into skin tissue. Under such conditions, it is not easy to capture enough biomarker to see using the traditional test.
But the team has a kind of secret weapon: “plasmonic-fluors”, an ultra-bright fluorescence nanomarker. Compared to traditional fluorescent markers, when a test was performed on a microneedle patch using plasmonic-fluorine, the target protein biomarker signal shone approximately 1400 times brighter and became detectable even when present at low concentrations. .
“Previously, the concentrations of a biomarker had to be on the order of a few micrograms per milliliter of fluid,” said Zheyu (Ryan) Wang, Singamaneni lab graduate student and one of the lead authors of the paper. It is well beyond the physiological range of the real world. But using plasmonic-fluoride, the research team was able to detect biomarkers on the order of picograms per milliliter.
“These are orders of magnitude more sensitive,” Wang said.
These patches have a multitude of qualities that can have a real impact on medicine, patient care and research.
They would allow providers to monitor biomarkers over time, which is especially important when it comes to understanding how immunity plays out in new diseases.
For example, researchers working on COVID-19 vaccines need to know if people are making the right antibodies and for how long. “Let’s put on a patch,” Singamaneni said, “and see if the person has antibodies to COVID-19 and at what level.
Or, in an emergency, “When someone complains of chest pain and they are taken to the hospital in an ambulance, we hope the patch can be applied right away,” Jingyi said. Luan, a recent graduate student. from the Singamaneni laboratory and one of the main authors of the article. Instead of having to go to the hospital and have blood drawn, paramedics could use a microneedle patch to test for troponin, the biomarker that indicates myocardial infarction.
For people with chronic conditions that require regular monitoring, microneedle patches could eliminate unnecessary trips to the hospital, saving money, time and discomfort – a lot of discomfort.
The patches are almost painless. “They penetrate about 400 microns deep into the skin tissue,” Singamaneni said. “They don’t even touch the sensory nerves.”
In the laboratory, the use of this technology could limit the number of animals needed for research. Sometimes research requires several successive measurements to capture the ebb and flow of biomarkers – for example, to track the progression of sepsis. Sometimes that means a lot of small animals.
“We could drastically reduce the number of animals required for such studies,” Singamaneni said.
The implications are vast – and Singamaneni’s lab wants to make sure they’re all explored.
There is a lot of work to be done, he said: “We will have to determine the clinical cut-offs,” which is the range of TFR biomarkers that corresponds to a normal or abnormal level. “We will have to determine which levels of biomarkers are normal, which levels are pathological.” And his research group is working on delivery methods for long distances and harsh conditions, offering options to improve rural health care.
“But we don’t have to do all of this ourselves,” Singamaneni said. Instead, the technology will be made available to experts in different fields of medicine.
“We have created a platform technology that anyone can use,” he said. “And they can use it to find their own biomarker of interest.”
This research was funded by the National Science Foundation (CBET-1900277) and the National Institutes of Health (R01DE027098, R56DE027924, R01CA141521, R21DA036663, R21CA236652).
The McKelvey School of Engineering at the University of Washington in St. Louis promotes independent inquiry and education with an emphasis on scientific excellence, innovation and collaboration without borders. McKelvey Engineering has leading research and graduate programs in all departments, particularly in Biomedical Engineering, Environmental Engineering, and Computer Science, and has one of the most selective undergraduate programs in the country. With 140 full-time faculty, 1,387 undergraduates, 1,448 graduate students and 21,000 living alumni, we work to solve some of society’s greatest challenges; prepare students to become leaders and innovate throughout their careers; and be a catalyst for economic development for the Saint-Louis region and beyond.
[ad_2]
Source link