
[ad_1]
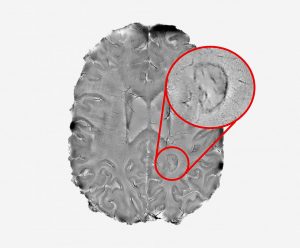
Brain lesions appearing as dark spots, "brooded" on imaging scanners, representing active inflammation, may be the mark of more aggressive and disabling forms of multiple sclerosis (MS), report researchers at National Institutes of Health (NIH).
With the aid of a powerful MRI brain scanner and a 3D printer, the team visualized brain images of nearly 200 multiple sclerosis patients and discovered that these spots – identified as chronic active lesions – could be used to alert people at higher risk of more aggressive and progressive forms of cancer. disease.
The studyAssociation of Chronic Activated Lesions of Multiple Sclerosis With In Vivo Disability"Was published in the newspaper JAMA Neurology.
"We discovered that it was possible to use brain scans to detect patients most susceptible to the most aggressive forms of multiple sclerosis. The longer the patient has active chronic lesions, the more likely they are to contract this type of MS, "said Daniel S. Reich, MD, Ph.D., lead author of the study and a senior NIH investigator, Press release.
"We hope these results will help test the efficacy of new treatments for this form of MS and reduce the suffering of patients," Reich added.
Previously, chronic active lesions could only be detected by autopsy. However, Reich and his team had shown in previous work that the examination of the brain of a living person using a powerful 7 Tesla MRI scanner could accurately capture these lesions by their darkened outer edges. .
"Finding a way to spot active chronic lesions was a big step forward and we could not have done it without the high power MRI scanner provided by the NIH. This then allowed us to explore the evolution of MS and its role in progressive MS, "said Martina Absinta, MD, Ph.D., director of the study and postdoctoral fellow in the Reich lab.
The team examined the brains of 192 multiple sclerosis patients participating in a trial conducted at the NIH Clinical Center. They found that 117 of them (56% of the initial study population) had at least one edge injury regardless of previous or current treatment.
Further analysis showed that 84 patients (44%) had no rim, 66 (34%) had one to three rims and 42 (22%) had four or more rim lesions.
Patients with four or more surrounding lesions continued to have motor and cognitive impairment at an earlier age and were 1.6 times more likely to be diagnosed with progressive MS than those without circled lesions.
By analyzing parts of the brain, the researchers also found that those with lined lesions had smaller brain volumes, less white matter, and smaller basal ganglia – structures deep in the brain that are associated with various functions, such as voluntary motor movements, cognition and emotion.
In a group of patients whose brains were scanned each year for at least 10 years, lesions without dark edges were found to shrink (3.6% reduction per year), while lesions with lesions remained large. stable or increased (2.2% per year).
"Our findings indicate the possibility of using specialized brain scans to predict who is at risk of developing progressive MS," said Reich.
The team also used a 3D printer to compare the lined spots found on the scans with those taken from the brain of a progressive MS patient who died during the study.
By examining these samples under the microscope, the scientists found that all the growth-scarred spots previously detected by scanning had the distinguishing features of chronic active inflammation.
"Our findings support the idea that active chronic lesions are very damaging to the brain," Reich said. "We must attack these lesions as soon as possible.
"The fact that these lesions are present in patients receiving anti-inflammatory drugs that calm the body's immune system also suggests that the field of MS research may want to focus on new treatments that target the immune system's unique immune system. brain – especially a type of brain cell called microglia, "he added. "At NIH, we are actively seeking patients who wish to participate in such studies."
Reich and his team have openly shared instructions for programming conventional MRI scanners found in most clinics to detect terminated active lesions.
These studies were funded by the NINDS intramural research program, the National Multiple Sclerosis Society, and the Conrad N. Hilton Foundation.
Ana is a molecular biologist passionate about discovery and communication. As a science writer, she seeks to connect the public, especially patients and the health community, with clear and quality information about the latest medical advances. Ana holds a PhD in biomedical sciences from the University of Lisbon, Portugal, where she specialized in genetics, molecular biology and infectious diseases.
[ad_2]
Source link