
[ad_1]
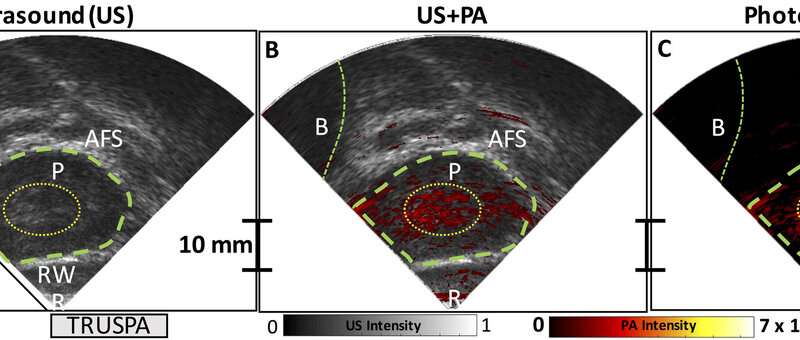
Scientists have used TRUSPA to image the prostate (P) in a patient with prostate cancer by combining ultrasound and photoacoustic approaches. Credit: S.R. Kothapalli et al., Science Translational Medicine (2019)
It is essential to observe the prostate closely to detect cancer, but its rather intimate position (just in front of the rectum) makes it difficult to visualize. Now professor and director of radiology in Sanjiv "Sam" Gambhir, MD, Ph.D., thinks he has a solution: a newly designed hybrid camera.
Traditionally, prostate cancer is detected via blood biomarkers associated with prostate cancer, such as the prostate-specific antigen (PSA). Doctors also often use ultrasound or magnetic resonance imaging (MRI) to look for physical changes to the prostate tissue. New techniques that exploit positron emission tomography (PET) can even capture molecular detail, but these tactics are relatively more expensive and use radiation, said Gambhir.
"But the problem is that prostate cancer often causes no anatomical changes until it is large enough or that it has spread beyond the prostate capsule into the lymph nodes that surround it, "said Gambhir. "Thus, for decades, we looked for ways to analyze and image the prostate in more detail in order to detect changes earlier, safely and at a relatively low cost."
The new technology of Gambhir, called TRUSPA (ultrasound and transrectal photoacoustic device), combines ultrasound and photoacoustic imaging techniques to simultaneously produce an image showing the anatomy of the prostate, functional details on the gland and Molecular information that can help mark cancerous tissue.
In a proof-of-principle study, Gambhir and a team of Stanford scientists, including biologists, engineers and physicians, demonstrated the value of the instrument in about 20 patients. An article describing the technology and results published in Science Translational Medicine. Gambhir is the lead author of the study and Sri-Rajasekhar Kothapalli, Ph.D., is the lead author.
Since ultrasound is already widely used by urologists and generally in human imaging, Gambhir chose to start with this as the foundation of TRUSPA. Generally, if a biomarker such as PSA is elevated in the blood of a patient, the doctors then turn to a combination of ultrasound and biopsy, during which they use a needle to draw about 20 samples from different regions of the prostate. This technique is rooted in a poke-and-hope theory because if you hope that you sample the part of the prostate that contains the cancerous tissue. But this is not guaranteed.
TRUSPA takes a different approach, which incorporates an imaging agent that cancer cells absorb easily – more than ordinary tissue. Then, thanks to photoacoustic molecular imaging (which monitors the absorption of light waves to help characterize the type of tissue), doctors can see where the cancer cells are in the prostate. The presence of the imaging agent in the tumor tissue alters the way the light is absorbed and the ultrasound waves are returned to the device, making it a kind of flag for the cancerous tissue.
"We opted for an imaging agent that was not specific to prostate cancer, but rather to cancerous tissue for our proof of concept," said Gambhir. This imaging agent was already approved by the FDA, which made it an easy starting point. "But the idea now is to improve accuracy by using a molecular-targeted photoacoustic molecular imaging agent that specifically binds to prostate cancer cells."
In the pilot study, scientists used the device in 20 people diagnosed with prostate cancer, looking to see if their device could also detect the disease.
"Not only have we been able to better understand the limitations of TRUSPA imaging in patients, but we have also probably observed tumors that would otherwise have been invisible to conventional prostate ultrasound," said Gambhir.

Credit: Stanford University
In one patient, they were even able to differentiate between malignant and non-cancerous cancerous tissues, which was then confirmed by further molecular analysis when the diseased prostate was removed from the patient. Gambhir warns that it is still a pilot project and that the team needs to test the imaging system a lot more before concluding that TRUSPA can operate this type of differentiation. In General. But it's a promising start, he said.
With clear evidence that the concept and technology can work in humans, Gambhir and his team continue to improve the device, its spatial resolution, molecular photoacoutique agents specific to cancer of the prostate and more, to improve the accuracy and sensitivity of signals. tumor detection.
"We are now starting to explore TRUSPA to also detect ovarian cancer, thyroid cancer and skin cancer," said Gambhir.
Butrus (Pierre) Khuri-Yakub, Ph.D., professor of electrical engineering at Stanford, Geoffrey Sonn, MD, assistant professor of urology, Joseph Liao, MD, associate professor of urology and James Brooks, MD, professor of urology, also contributed to the project.
Study Shows More Effective Method For Detecting Prostate Cancer
Sri-Rajasekhar Kothapalli et al. Simultaneous transrectal ultrasound and photoacoustic imaging of the human prostate Translational medicine science (2019). DOI: 10.1126 / scitranslmed.aav2169
Quote:
Prostate Imaging Camera Captures Molecular Details to Detect Cancer (August 29, 2019)
recovered on August 29, 2019
on https://medicalxpress.com/news/2019-08-prostate-imaging-camera-captures-molecular-cancer.html
This document is subject to copyright. Apart from any fair use for study or private research purposes, no
part may be reproduced without written permission. Content is provided for information only.
[ad_2]
Source link