[ad_1]
Researchers have found intriguing evidence in mice that a blood-brain pathway could be responsible for introducing the toxic particles that contribute to Alzheimer’s disease into our gray matter.
This work is still in its early stages and we are a long way from being able to apply it to humans, but it is a compelling lead that could help us finally explain why the cause of degenerative disease has proven so difficult to determine. and process.
Decades of detective work have made the beta-amyloid protein fragment the main villain in the development of dementia, Alzheimer’s disease.
Despite its reputation, there is still a lot that we don’t understand about this short chain of amino acids and its usual role in the body. What we do know is that if it forms clumps in the brain, the long-term prognosis for mental health is not good.
The arguments against beta-amyloid, however, are not entirely clear.
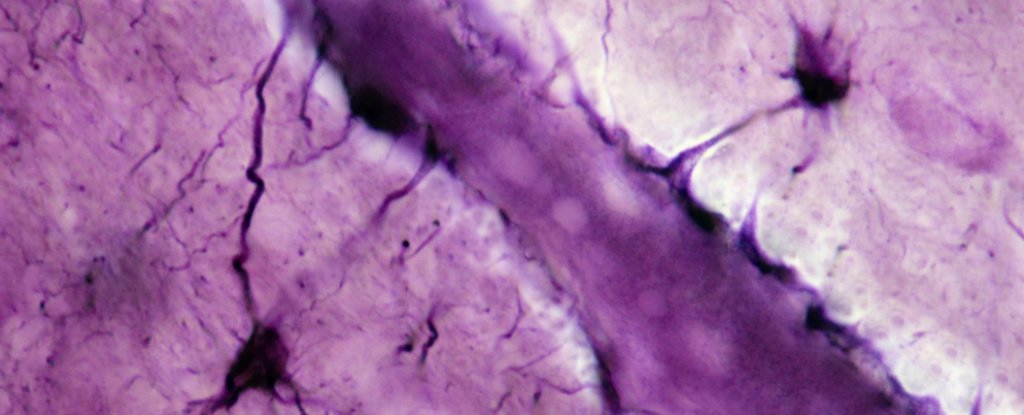
Much has been discovered in recent years about its movement throughout the body and in the brain and how its presence ends up killing neurons. But nagging questions remain, such as why therapies targeting beta-amyloid plaques fall short of expectations.
One continuing area of interest does not focus on plaques but on the relationship between beta-amyloid and a class of fat-transporting chemicals called lipoproteins.
Using a transgenic mouse model, researchers at the Curtin Health Innovation Research Institute in Australia have found compelling evidence that beta-amyloid proteins produced elsewhere in the body are smuggled into the brain via this transport system. lipids.
“Our research shows that these toxic protein deposits that form in the brains of people with Alzheimer’s disease most likely infiltrate the brain from particles that carry fat in the blood, called lipoproteins,” explains the principal investigator and physiologist John Mamo.
“This ‘blood-to-brain pathway’ is important because if we can manage the blood levels of amyloid lipoproteins and prevent their leakage into the brain, it opens up potential new treatments to prevent Alzheimer’s disease and slow memory loss. “
The challenge for the researchers has been to figure out exactly how a small protein found throughout the body ends up building up in brain cells to such concentrations that it ultimately turns out to be fatal.
One possibility is that it is simply produced in large quantities inside the tissues of the brain. Yet having high concentrations of beta-amyloid in the peripheral blood is an exceptionally good predictor of the subsequent development of brain plaques.
One clue can be found in how a soluble version of low-density lipoprotein mops up about 70 to 90 percent of the beta-amyloid in human plasma. There is also evidence that the leakage of this fat transporter complex from capillaries deep inside Alzheimer’s brain characteristically damages blood vessels.
Follow-up studies based on mice have only suggested that there is some sort of link between lipoproteins and beta-amyloid. Rodents fed a diet high in saturated fat (the kind they would need lots of lipoproteins for) had the same leaky blood vessels in the brain, for example.
Still, the possibility that beta-amyloid could be generated inside the brain at toxic concentrations could not be ruled out as a contributing factor. Mamo and his team therefore designed mice that could only express key genes to build beta-amyloid in their liver.
That way, any Alzheimer’s-like pathology they could detect in the brain of the mouse models had to come from the supply of beta-amyloid from the outside.
“As we predicted, the study found that mouse models producing lipoprotein-amyloid in the liver suffered from inflammation in the brain, accelerated brain cell death, and memory loss,” explains Mamo.
While there is still a lot of work to be done, the discovery suggests that there may be therapies for Alzheimer’s disease that target the diet or use pharmaceuticals that manage how lipoproteins interact with beta. amyloid.
Aging populations around the world can expect an increase in the number of people with Alzheimer’s disease in the coming decades. At present, it is believed that more than 30 million people suffer from this debilitating disease.
The more we learn about the operations of beta-amyloid as it moves through our bodies, the better our chances of finding early ways to diagnose, treat, or even prevent the loss of neurological function that impacts so many lives.
This research was published in PLOS Biology.
[ad_2]
Source link