[ad_1]
Over the last 25 years, scientists have fought Alzheimer's disease under one guiding principle: Amyloid beta amyloid deposits deposited outside sensitive brain cells progressively damage neuronal functions and cause memory loss. The solution seems simple: eliminate unwanted amyloid, protect the brain.
They could be completely wrong.
Last month, Alzheimer's defeated another market-leading drug that was trying to prevent or eliminate amyloid deposits, adding to the "dream graveyard" of the disease. Although the drug suppresses toxic amyloid, patients have not improved. Failure again leads scientists to face an uncomfortable truth: targeting amyloids when patients already have symptoms of memory does not work. Eliminate soluble amyloid – protein fragments before they aggregate into junk – also dead ends.
It's time to think outside the box.
Last week in Nature NeuroscienceDr. Mark Mattson's team of the National Institute on Aging's intramural research program has provided substantial evidence that the senolytic, gold-bearing anti-aging drugs, save losses of memory in Alzheimer's disease, at least in mice genetically engineered to accumulate amyloids in their brains.
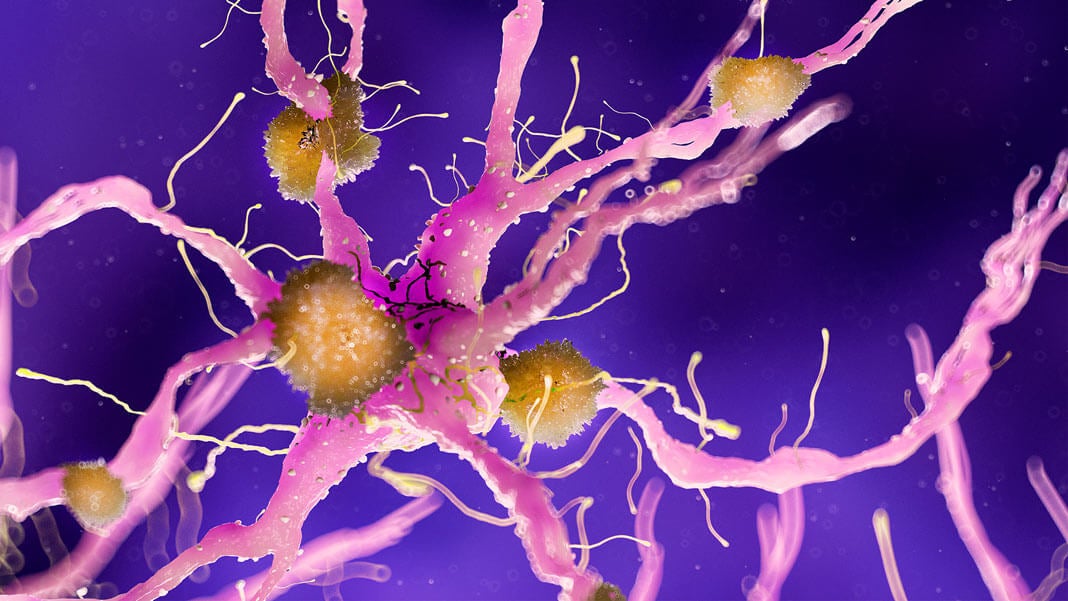
With age, toxic proteins have damaged a particular type of brain cell called OPC, turning them into cellular monsters that cause inflammation of the brain. These zombie cells dump "toxic" molecules into their local environments, turning essential parts of the brain into tiny, infernal landscapes that, like overheated processors, reduce the efficiency of the calculations.
After weekly treatments with drugs for just three months, the team found fewer zombie OPC cells clustered around amyloid clusters in the brains of the mice. The treatment also disintegrated the masses in the memory-related regions and, perhaps more importantly, the brains were no longer inflamed. In a series of memory tests, treated mice regained their ability to learn and memorize complex labyrinths.
"Our results pave the way for future preclinical and clinical studies that will test the hypothesis that senolytic treatments can … preserve brain function in [Alzheimer’s] and other age-related neurodegenerative disorders, "the authors concluded.
What are senolitics?
Three years ago, in a laboratory of the Mayo Clinic, Drs. Darren Baker and Jan van Deursen were speechless in front of the cages of old, healthy and playful mice, wandering home like zealous teenagers. At the time, the team had no idea they were about to start an anti-aging revolution.
The mice had received powerful rejuvenating drugs called senolytics. In general, senolytics constitute a large family of drugs with multiple origins. Some have been developed originally to destroy cancer cells. Others came from fruits and vegetables. Shockingly, when administered to older animals, the senolytics effectively hunted stubborn zombie cells while sparing those in good health.
Zombie cells are aging cells that can no longer perform their functions effectively but refuse to withdraw. Rather than giving in to the younger generation, these senescent cells struggle to stay alive, letting out molecules that increase inflammation in their environment. Older tissues already suffer from long-term negative inflammations, which is tantamount to saying that the body turns its molecular protective bazookas towards itself. The zombie cells pour gasoline on this fire.
Until now, senescent cells are linked to aging of the brain, muscles, hair and heart. Their reference sheet is the preferred target of scientists to prevent tissue damage with age, or to extend their life.
If you think "duh, of course drugs that help with aging also help Alzheimer's disease, which is unfortunately quite rare. Normal aging and Alzheimer's disease are completely different in the brain. For example, normal aging does not kill neurons; Alzheimer's doing. This is why scientists do not always confuse what they have learned from the aging brain with that of Alzheimer's disease.
But there are exceptions.
The senolytic connection
Mattson decided to make a leap of faith.
Because the senolytics clearly help the aging brains, his team decided to examine whether these drugs also stimulate brain function during the accumulation of amyloid substances. The team designed mice with a genetic mutation that increased beta-amyloid deposition in their brains as they grew older. Some mice also had an additional mutation that shone senescent cells in neon green under fluorescent light, allowing the team to track these cells and discover their identity.
Remarkably, these are not neurons that have turned into zombies. The brain's immune cells, called microglia, have also prevented the curse of senescence. Beta-amyloid rather exercised its black magic on OPC, which progressively hurt with age and "settled" with amyloid clusters. Under the microscope, senescent OPCs gathered around these tufts as witches around a cauldron and spat inflammatory molecules to injure their neighbors.
It's a story of good cells that went wrong. Normally, OPC belong to a family of "guardian angel" cells that protect and support neuronal function. They activate in response to a brain injury to repair the electrical insulation sheath that encapsulates the neurons. Without OPC, the cabling of our brain loses its insulating layer and the brain functions suffer.
Here are the cases where senolytics comes in. The DQ combo (alas, not the Dairy Queen but the less intuitive duo dasatinib and quercetin) has already been approved by the FDA as "senolytic" compounds because of its ability to eliminate senescent cells from aging or damaged tissues. . The team injected the drug cocktail into their Alzheimer mice once a week for 11 weeks.
The positive results were rapid: beta-amyloid levels in the mouse dropped in three months. In addition, the treated mice had fewer senescent cells in their hippocampus, the main center of brain memory, and navigated better in complex aquatic labyrinths than their peers.
Outside the box
Given the atrocious therapeutic results of Alzheimer's, the Mattson study does not prove much in itself: it is a study, in a type of Alzheimer's model that captures only part of the pathology of Alzheimer's disease. disease.
But add a dose of previous evidence, and a trend is bubbling. In 2018, Baker and van Deurson, the first senolytic researchers for brain health, discovered that these drugs also helped preserve the memory of mice with another type of protein accumulation – the tau – that is present in the brain Alzheimer's disease in mice.
In their study, by intelligently destroying senescent cells (no longer neurons but star-shaped glia) using genetic techniques or drugs, the team protected vulnerable neurons from the hippocampus and cortex and stimulated memory. Around the same time, Dr. Miranda Orr of the University of Texas Health Sciences Center also discovered that senescent cells – this time neurons – were associated with an abnormal accumulation of protein in the brain resembling Alzheimer's disease in mice.
Unlike these previous studies, the Mattson team found no abnormalities in neurons or star-shaped glia. Confused? Yeah, that's the mystery of Alzheimer's disease: As animals do not normally develop the disease, scientists need to rely on different genetic models to force the symptoms in mice. The caveat is that DIY at the DNA level does not completely recapitulate the complexities of Alzheimer's disease and we end up with conflicting and sometimes complementary data.
"The role of senescent cells in most human diseases, including Alzheimer's disease, is not known. We did not look for long-term negative effects of senolysis on the mouse brain. The potential impact could be significant, but we need to be cautious, "Baker said. Singularity Hub.
Together, the three studies make clearly show that senolytics have a positive effect on the Alzheimer's brain in the short term – regardless of cell type.
At least in the mouse. Baker warned: "It's important to keep an open mind about what can happen when strategies are used in individuals, because poorly designed or controlled studies could pose problems in interpreting the results of these studies."
Nevertheless, it is good to get out of the tunnel vision of beta-amyloid: as other ideas gain ground, a long-awaited advance could occur. For example, some scientists believe that the blood components of young donors might be the answer. Some people think that tinkering with brain waves could be the cure. Others hope to directly modify the genetic links with the disorder.
In the end, it's about helping around 50 million people around the world suffering from Alzheimer's disease, and that number is increasing every day. Each. Drive. Account. And senolytics are promising.
Image Credit: Sebastian Kaulitzki / Shutterstock.com
[ad_2]
Source link