[ad_1]
By
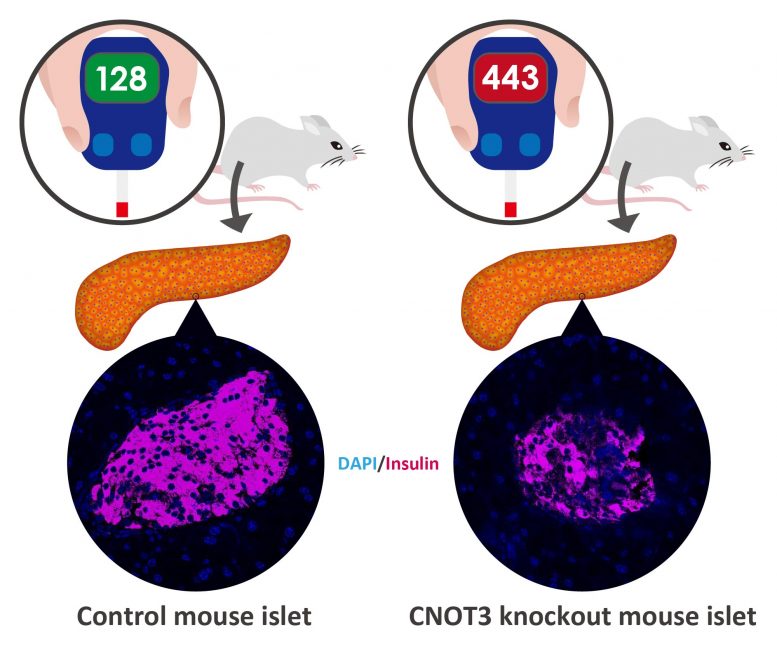
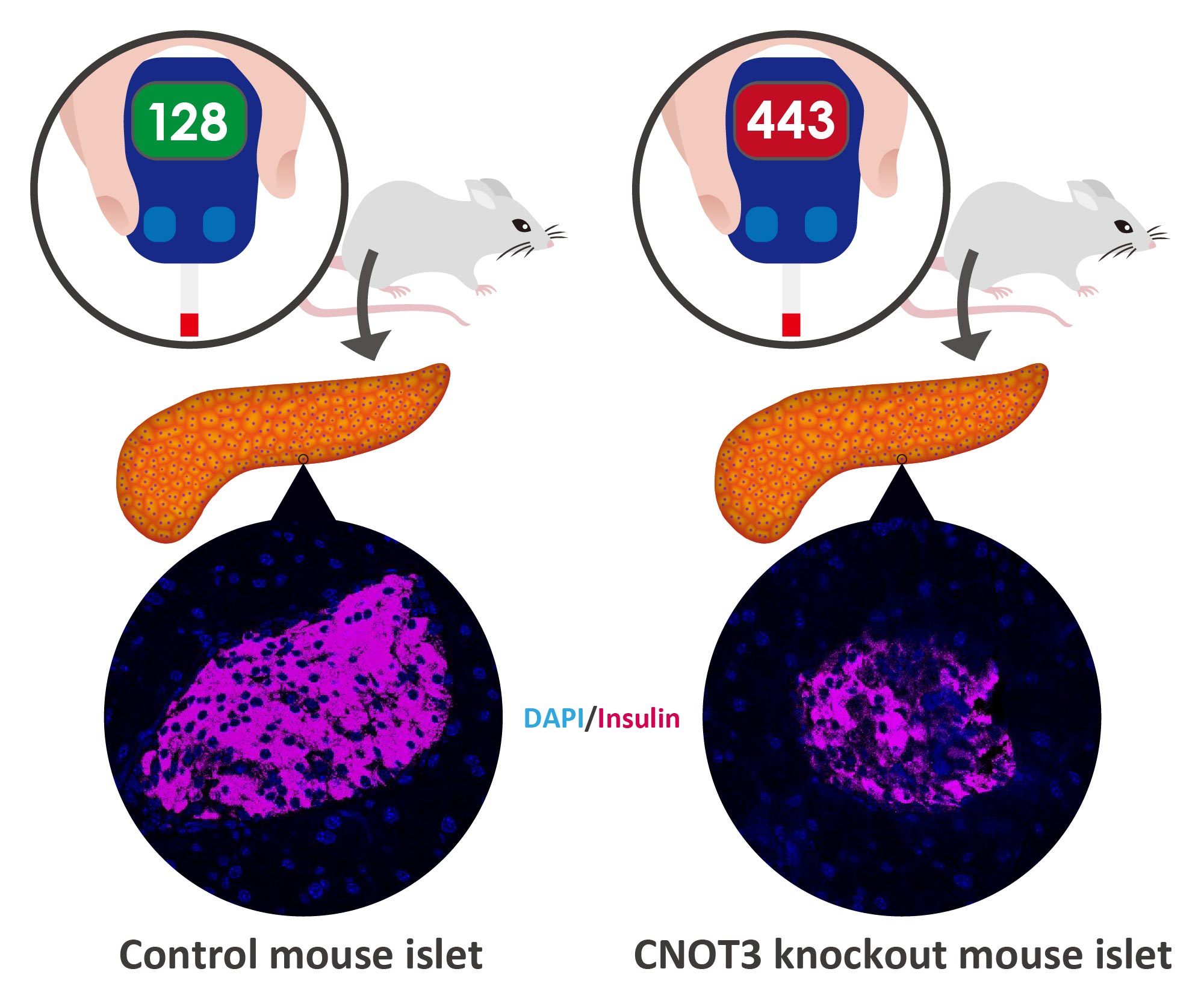
Mice lacking CNOT3 in pancreatic beta cells have fewer insulin-producing cells, which leads to diabetes. Credit: OIST
A protein common throughout the body plays a key role in regulating glucose levels, according to new research from the Cell Signal Unit at the University of Okinawa Institute of Science and Technology Graduate University (OIST) and the Riken Center of Integrative Medical Sciences. Called CNOT3, this protein has been shown to silence a set of genes that would otherwise cause insulin-producing cells to malfunction, which is linked to the development of diabetes.
Diabetes is a common disorder that causes very high blood glucose levels. If left untreated, it can lead to serious health problems like kidney failure, heart disease, and vision loss. This disorder occurs when there is not enough insulin in the body or when insulin-induced responses are weakened. Insulin normally lets glucose enter cells for energy consumption and therefore, without it, glucose builds up in the bloodstream instead. A lack of insulin is often due to the fact that pancreatic beta cells, which normally synthesize and secrete insulin, have stopped working properly.
“We know that beta cell defects can lead to high blood glucose levels and eventually diabetes.” said Dr Dina Mostafa, former doctoral student of the Unit and first author of the article published in Communications biology. “Our results suggest that CNOT3 has a role to play in this area and plays a key role in maintaining normal beta cell function.”
Knocking out CNOT3 leads to diabetes in mice:
CNOT3 is a jack of all trades. Many organs throughout the body express it and regulate different genes in different tissues. But its activity has a common basis: it helps to keep cells alive, healthy and functioning properly. It does this through several different mechanisms, such as making the right proteins or removing certain genes.
Here, the researchers studied its function in islet cells of pancreatic tissue in mice. These islets are notoriously difficult to work with, occupying only one to two percent of the pancreas, but they are where the beta cells are.

Researchers from the OIST Cellular Signal Unit. From left to right, Dr Akiko Yanagiya, Dr Dina Mostafa and Professor Tadashi Yamamoto. Credit: OIST
The researchers first investigated whether CNOT3 expression differed in diabetic mice compared to non-diabetic mice. Looking at these islets, they found that there was a significant decrease in CNOT3 in diabetic islets compared to non-diabetics.
To study the protein’s function in more detail, the researchers blocked its production in the beta cells of otherwise normal mice. For four weeks the animals’ metabolism was functioning normally, but by week eight they had developed glucose intolerance and at 12 weeks had full-blown diabetes.
Without CNOT3, the researchers found that certain genes, which are normally turned off in beta cells, turn on and start producing proteins. Under normal circumstances, these genes are silenced because once they are turned on they cause all kinds of problems for beta cells, like preventing them from secreting insulin in response to glucose.
“We still don’t know much about these types of genes, such as their normal function and the mechanism involved in silencing them,” Dr Mostafa said. “So, it was very gratifying to see that CNOT3 was a big factor in keeping them turned off.”
The messenger RNA link:
Further research into the cellular mechanisms behind this found a surprising link between CNOT3 and the messenger RNA of these normally disabled genes. A messenger RNA (mRNA) is a single-stranded molecule that matches the genetic sequence of a gene and is essential for protein synthesis.
Under normal circumstances, the mRNA for these genes is barely expressed. But once CNOT3 was removed, the researchers found that the mRNA was much more stable. In fact, the protein was produced from stabilized mRNA, which has adverse effects on normal tissue function. This suggests that at least one way these genes are kept turned off is the destabilization of their mRNA, driven by CNOT3.
“This study is a step towards understanding the molecular mechanisms that govern the normal functioning of beta cells,” said Dr. Mostafa. “Ultimately, this could contribute to new ways of preventing and treating diabetes.”
###
Reference: “Loss of β cell identity and diabetic phenotype in mice caused by disruption of CNOT3-dependent mRNA deadenylation” by Dina Mostafa, Akiko Yanagiya, Eleni Georgiadou, Yibo Wu, Theodoros Stylianides, Guy A. Rutter, Toru Suzuki and Tadashi Yamamoto, August 28, 2020, Communications biology.
DOI: 10.1038 / s42003-020-01201-y
Alongside Dr Mostafa, the research group included Dr Akiko Yanagiya and Professor Tadashi Yamamoto from the Cell Signal Unit at OIST, Dr Eleni Georgiadou and Professor Guy A. Rutter from Imperial College London, Dr Yibo Wu and Dr Toru Suzuki from the Riken Center of Integrative Medical Sciences, and Dr Theodoros Stylianides from Loughborough University.
[ad_2]
Source link