[ad_1]
Utah doctors are doing what they say is the equivalent of rationing care. Minnesota’s intensive care beds are almost full. And the country as a whole continues to break hospitalization records – all as millions of Americans travel to spend Thanksgiving with friends and family.
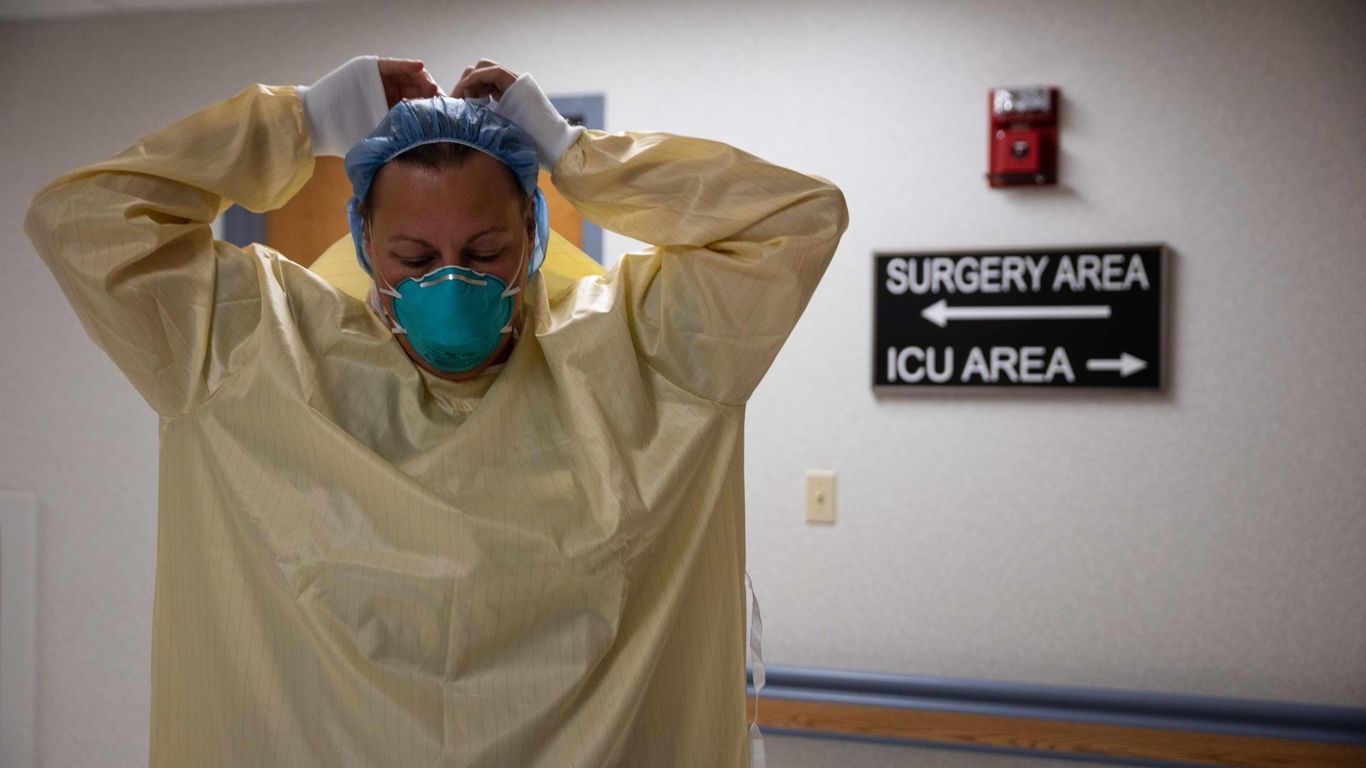
Why is this important: America’s healthcare workers are exhausted and the sickest coronavirus patients aren’t getting the kind of care that could be the difference between living and dying.
The big picture: Some overwhelmed hospitals send patients for care elsewhere, while others reduce the quality of care their patients receive – a byproduct of staff shortages.
- For example, 75% of Kansas and Missouri counties do not have intensive care beds, so these patients are being sent to city hospitals – some of which are starting to cringe under the increasing number of cases, reports NPR.
- “It is not only the rural health care infrastructure that is overwhelmed when there are not enough hospital beds, it is also the surrounding neighborhoods, the suburbs, the infrastructure of urban hospitals begins. also to become overwhelmed, ”Shannon Monnat, rural health researcher at Syracuse University, told NPR.
What they say: “There are things happening right now that wouldn’t normally happen,” Andy Pavia, chief of pediatric infectious diseases at the University of Utah, told the Salt Lake Tribune.
- “Idaho patients are not accepted. People stay in small community hospitals rather than going to referral hospitals, where the largest [technical] sophistication is. Now is just not the time when people are piled up in bedless hallways. “
The bottom line: Healthcare workers are one of the country’s most limited resources in our fight against COVID. In too many places they are reaching their full capacity.
Go further: U.S. coronavirus hospitalizations continue to break records
[ad_2]
Source link