[ad_1]
Depression can be a terribly relentless condition. Fortunately, researchers around the world are constantly working on new treatment options, like a newly designed brain implant for resistant depression.
In total, up to a third of people with depression do not respond or become resistant to treatment. No type of medication or therapy seems to help. For those suffering from such treatment-resistant depression, the future may seem particularly bleak.
This is what happened to Sarah, a 36-year-old woman who has suffered from severe depression and resistant to treatment since she was a child. But a new proof of concept intervention has brought significant relief to Sarah and may offer hope to many like her. The only problem? This requires a tailor-made “brain stimulator” for each person.
“I was on the phone,” said Sarah, who asked to be identified only by her first name.
“I was severely depressed. I couldn’t see myself going on if that was all I could do, if I could ever get past that. It wasn’t a life worth living. lived. “
Fortunately, Sarah was able to participate in a case study with a neuroscience research team at the University of California, San Francisco (UCSF); the team’s project was to study deep brain stimulation methods that could potentially alleviate symptoms of depression.
While the idea of having a small device implanted in our skulls may seem terrifying to some, deep brain stimulation has been successful in other brain disorders such as Parkinson’s disease and epilepsy.
But depression is much more complicated than either of these conditions. So far, results on deep brain stimulation for depression that target particular regions of the brain – such as Brodmann’s area 25 – have been mixed and mostly disappointing.
However, the UCSF team has made a significant change to this type of therapy.
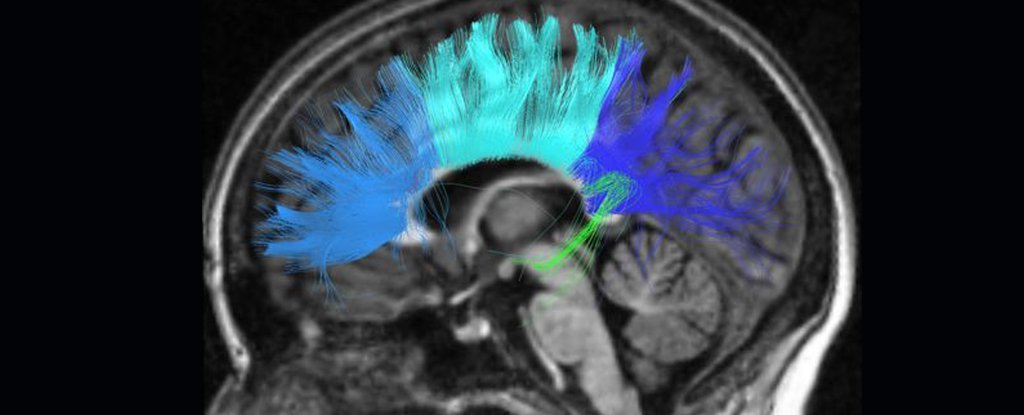
Instead of applying the same brain stimulation treatment for everyone, the researchers manually tracked where Sarah’s depression was appearing in her brain. They identified a biomarker – in this case, a specific brain wave pattern – that had never been identified in major depressive disorder before, and used it to customize the machine to only stimulate when and where the biomarker was expressed.
The team placed an electrode wire in the area of the brain where the biomarker was found, and a second where Sarah’s “vacuum circuit” was located. The best location for symptom relief took some time to figure out; once inserted, the first wire would detect the biomarker, and the second would produce a tiny amount of electricity for six seconds deep in the brain region.
 (Ken Probst / UCSF)
(Ken Probst / UCSF)
Above: The device with one wire (blue) in the amygdala to detect the biomarker, and the other (red) in the ventral capsule for stimulation.
“The effectiveness of this therapy showed that not only did we identify the right brain circuit and the right biomarker, but we were able to replicate it at an entirely different later phase of the trial using the implanted device,” said the first author, UCSF psychiatrist Katherine. Scangos.
“This success in itself is an incredible advance in our understanding of the brain function that underlies mental illness.”
Now we really have to point out that this new successful result has only been achieved in one patient so far. There have been a lot of other studies on deep brain stimulation that haven’t come to fruition in trials, and we don’t yet know how this approach will fare over time.
But for Sarah, the changes have been immense.
“In the first few months the depression abated so sharply and I wasn’t sure it would last,” she said.
“But it lasted. And I realized that the device really increases the therapy and self-care that I learned.”
 Sarah in her garden. (John Lok / UCSF 2021)
Sarah in her garden. (John Lok / UCSF 2021)
Interestingly, stimulating the brain only after symptoms – or in this case the biomarker – appear is also a new way to use deep brain stimulation in depression. In previous studies, stimulation was done continuously at predefined intervals, not when specific depressive brain activity occurred. That in itself could be a huge change to make the technique more efficient.
But this biomarker is most likely not universal, which means researchers will need to find the individual version of Sarah’s biomarker for each patient so that they can be treated the same.
The team is already recruiting more patients into the study to see if they can find more personalized depressive markers and provide them with their own specialized “brain stimulator.”
“We need to look at how these circuits vary from patient to patient and repeat this work multiple times. And we need to see if an individual’s biomarker or brain circuit changes over time as treatment continues. “said Scangos.
This is the very beginning of a treatment design, and there will be many challenges ahead before this becomes a potential option for patients outside of the research setting. But for people with treatment-resistant depression, this personalized treatment could one day be an exciting way forward.
“We have developed a precision medicine approach that has been successful in managing our patient’s treatment-resistant depression by identifying and modulating the circuit in her brain that is uniquely associated with her symptoms,” said one of the members. the UCSF team, psychiatric researcher Andrew Krystal.
“This study points the way to a new paradigm that is desperately needed in psychiatry.”
The research was published in Natural medicine.
[ad_2]
Source link