[ad_1]
The United States Food and Drug Administration (FDA) has approved siponimod (Mayzent, Novartis) to treat adults with relapsing forms of multiple sclerosis (MS), including a clinically isolated syndrome, relapsing-remitting disease, and an active secondary progressive disease (OS), the agency said.
"Multiple sclerosis can have a profound impact on a person's life," said in a statement Dr. Billy Dunn, director of the division of neurology products at the Center for Evaluation and Research of FDA drugs. "We are committed to continuing to work with companies that are developing additional treatment options for multiple sclerosis patients."
The approval was based on the results of the EXPAND Phase 3 study, which randomly assigned 1651 patients with MSPS who had an extended disability status scale score of 3.0 to 6.5. and oral siponimod 2 mg once daily (1,105 patients) or placebo (546 patients) up to 3 years of age or until the onset of a predetermined number of months. confirmed events of change in disability.
Initially, the average time since onset of the first symptoms of multiple sclerosis was 16.8 years and the average time since conversion to SPMS was 3.8 years; 64% of the patients had not relapsed in the last 2 years and 56% needed help with walking.
The primary endpoint was the confirmed 3-month disability progression time. This occurred in 26% of patients treated with siponimod and 32% of those receiving placebo (risk ratio: 0.79, 95% confidence interval). [CI]0.65 – 0.95; relative risk reduction, 21%; P = 0.013).
Serious adverse events were reported in 18% of patients treated with siponimod versus 15% in the placebo group. Lymphopenia, increased hepatic transaminase concentration, early bradycardia and bradyarrhythmia, macular edema, hypertension, varicella zoster reactivation, and seizures occurred more frequently with siponimod than with siponimod. with the placebo.
Titration of the initial dose attenuated the effects of the first cardiac dose. The frequency of infections, malignancies and deaths did not differ between groups.
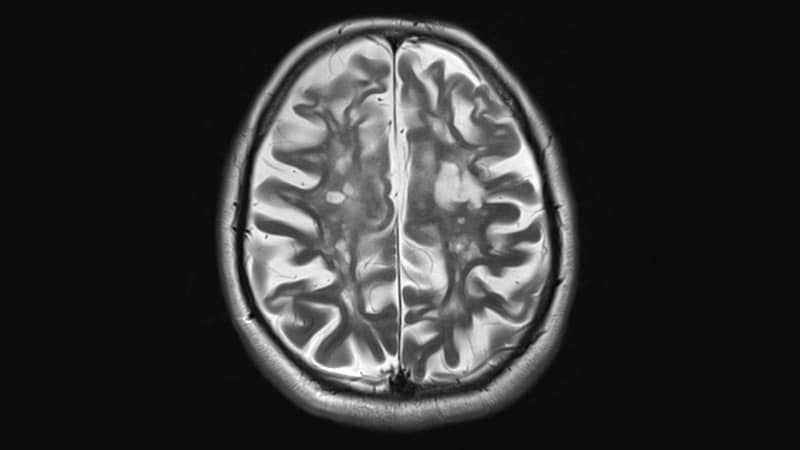
In addition, the secondary results of the trial suggest that the reduction in brain volume was less severe in treated subjects than in those receiving placebo (adjusted mean change in brain volume, -0.50% vs. -0.65%; difference between groups, 0.15% points [95% CI, 0.07 – 0.23 percentage points]; P = .0002).
However, siponimod did not have a significant effect on the walking speed of patients in the 25-foot timed walk test.
Subgroup analyzes favored siponimod over placebo throughout the previous disease duration, disability status, and age, although the effect of treatment became less pronounced with age, disability, the initial duration of the illness and the decrease in signs of disease activity.
The drug should be used along with a patient treatment guide describing "important information about the uses and risks of the drug," the release said. It has been shown that treatment increases the risk of infections. Therefore, a complete blood count should be performed prior to initiation of treatment. This could cause macular edema, "so patients should contact their doctor if they experience a change in vision, the FDA adds.
It can cause transient bradycardia or deterioration of lung function. Hepatic enzymes should be checked before starting the drug "and health professionals should closely monitor patients with severe liver failure," as well as blood pressure during treatment, the statement said.
Women of childbearing potential must use effective contraception during and for 10 days after stopping treatment because of the potential risk of fetal injury, the agency said. "Health professionals should monitor patients with reversible posterior encephalopathy syndrome and patients treated with immunosuppressants / immunomodulators because there may be an involuntary additive immunosuppression with" siponimod.
For more news, join us on Facebook and Twitter
[ad_2]
Source link