
[ad_1]
"Several studies have shown a correlation between increased bad density and the risk of bad cancer. It is multiplied by 2 to 5 depending on the density, "says Dr. Cutuli, radiation oncologist and president of the French Society of Senology and Mammary Pathology.
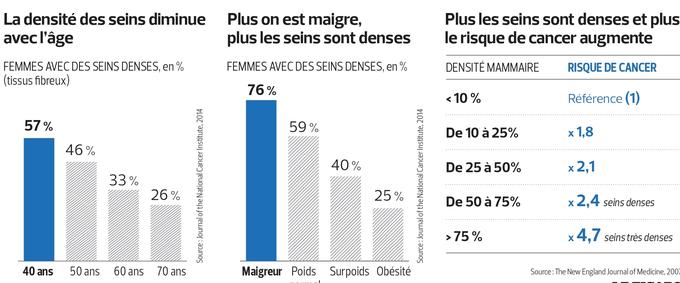
Your doctor may have already told you that you have dense bads and that you might need special monitoring? Indeed, it is a well-established cancer risk factor. It is even one of the most important after BRCA1 / BRCA2 gene mutations. "Several studies have shown a correlation between increased bad density and the risk of bad cancer. It is multiplied by 2 to 5 depending on the density (see infographic below from Mammographic Density and the Risk and Detection of Breast Cancer, NEJM, 2007, 356: 227-36), "says Dr. Cutuli, a radiotherapist and radiation oncologist. President of the French Society of Senology and Mammary Pathology
"It can not be guessed by mere palpation," he adds. Breast density is a radiographic criterion that reflects the proportion of fibrous tissue in the bads compared to fat tissue. "On a standard bad x-ray (mammogram), the glandular tissue (fat) appears in black when crossed by the X-rays, while the fibrous tissue, which stops them, appears in white. The problem is that bad cancers also appear in white.
Therefore, detecting cancer in a dense bad because of the fibrous tissue becomes particularly difficult. The radiologist usually clbadifies bad density in four levels, but software can also calculate it as a percentage of fibrous tissue. There are more dense bads in young women but also in skinny women. While there is an 85% chance that a conventional mammogram will detect bad cancer when it is present in a low-density bad, performance drops to around 62% -68% in a dense bad (mask effect).
MRI and ultrasound
This explains some of the failures of mammography. Before age 56, bad density probably plays a role in a significant proportion of bad cancers that go unnoticed despite participation in screening. Thus, half of the cancers detected in the year following a seemingly rebaduring mammogram occur in women with dense bads, whereas this is only the case for 17% of these cancers after 56 years.
When bads are dense and especially in case of other risk factors (family history, woman who has not had a pregnancy), this may justify using ultrasound and, sometimes, MRI as a supplement, rather than mammography, "says Dr. Cutuli. MRI and ultrasound are just some of the imaging tools used in the European MyPreBS study (My Personal Breast Screening), coordinated by Unicancer with financial support from the European Commission. The study has just been launched under the leadership of Dr. Suzette Delaloge, oncologist and head of the Breast Pathology Committee at Gustave-Roussy (Villejuif). "It's an interesting move that puts women into four different risk groups," says Dr. Cutuli. But the results will not be known for at least five years. "
Source link