
[ad_1]
As Philadelphia grapples with a deadly pandemic and its effects on the existing opioid crisis, research suggests black residents have been particularly affected by fatal overdoses since the emergence of COVID-19.
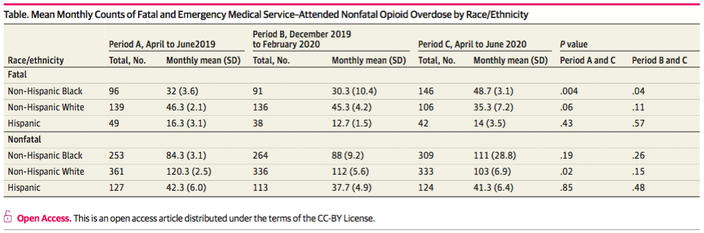
Fatal overdoses among black residents increased by more than 50% in the months following the decision to stay at home in Pennsylvania compared to the same time a year earlier. Overdose deaths among white residents declined markedly over the period.
Researchers at Penn Medicine analyzed trends in opioid overdoses released last year by the Philadelphia Department of Public Health and the Philadelphia Fire Department after seeing indications of an increase in deaths among black residents. Their findings mark a reversal of trends generally seen in the opioid epidemic.
“Philadelphia has been devastated by the opioid crisis, which was previously more acute in the white community,” said Dr. Utsha Khatri, emergency physician and lead author of the study, published in JAMA Network Open. “Recently, however, we have followed a disturbing trend towards higher rates of fatal and non-fatal overdoses among black residents of Philadelphia. These differential opioid overdose trends suggest that racial inequalities have been exacerbated by the pandemic. . “
The study looked at three distinct time periods:
• Period A – from April to June 2019
• Period B – From December 2019 to February 2020
• Period C – from April to June 2020
The researchers chose period C to coincide with the full months following the stay-at-home order, while period A offered a year-over-year comparison and period B provided an overview of the months leading up to the stay-at-home order. pandemic.
Overall, fatal overdoses remained relatively unchanged in Philadelphia in a year-over-year comparison between Period A and Period C. The city recorded an average of 94 overdose deaths per month during Period A and 98 deaths per month during period C.
But among blacks, overdose deaths have fallen from a monthly average of around 30 in Period A and B to around 49 in Period C.
Fatal overdoses among white Philadelphia residents fell from a monthly average of 46 and 45 in Periods A and B, respectively, to just 35 in Period C. This marked a 31% decrease from year to year. the other and a decrease of 22% compared to the pre-calendar period of the pandemic.
Among Hispanic residents, the average monthly number of deaths increased from about 16 to 12 in Period A through Period B, and then rose to around 14 in Period C.
Similar racial tendencies were detected among the non-fatal overdoses in Philadelphia.
 Open Source / JAMA Network
Open Source / JAMA Network
The Penn researchers published their demographics of opioid deaths in Philadelphia in the JAMA Network Open.
“The results of this study are sobering, “said lead author Eugenia South, assistant professor of emergency medicine at Penn.” The black community has been hit extremely hard since the start of the pandemic – both by the disease itself and by social and economic issues. fallout, which includes increased gun violence, job losses and the closure of small businesses. We believe that the increase in fatal and non-fatal opioid overdoses is a symptom of this. “
The study’s publication comes as the city’s health department grapples with the causes and changing demographics of the opioid epidemic.
Preliminary statistics for 2020 include a total of 950 deaths from January to September. Once all the information is recorded and verified, it is predicted that 2020 will be the deadliest year in the city for opioid overdoses.
Much of this has been attributed to the continued rise in the lethal synthetic opioid fentanyl, which increasingly appears in drug mixtures with methamphetamine, PCP, and cocaine, in addition to heroin. The health department warned this week that “fentanyl is in everything,” providing statistics on overdose deaths linked to fentanyl combined with other drugs in recent years.
Penn’s research team believe the increasing prevalence of fentanyl may partly explain why fatal overdoses have increased among black residents.
“How this has translated into an increase in accidental drug overdoses is unknown, but may be related, in part, to the purchase of more economical drugs from lesser known sources,” said the co-author of the study Kendra Viner, head of the substance use division in the health department. prevention. “We are concerned that fentanyl, a potent synthetic opioid that is cheaper to produce and distribute, is increasingly present in non-opioid drugs. This could put populations of drug users without prior exposure to opioids at a higher risk of overdose.
The researchers also hypothesized that access to opioid treatment remains inequitable. Buprenorphine, a prescribed drug used to quell opioid cravings, remains more available to white patients than to black patients.
And although research shows that drug use tends to be quite similar across races, blacks are more likely to face legal penalties for it. The treatment has not been effective enough to reach people who are already involved in the criminal justice system.
The study was limited to Philadelphia, but researchers believe that similar trends in opioid overdose deaths in other US cities may become evident with further analysis. The authors of the study recommend that health services publicly report opioid overdoses by race.
“Cities across the country need to examine overdose trends in various socio-demographic groups to have a more granular understanding of who is affected and how best to target response efforts,” Khatri said.
The health department is currently developing a community education initiative to raise awareness and prevent overdoses involving fentanyl drug mixtures. The program will include the distribution of test strips of fentanyl and naloxone, the anti-overdose drug used to counter the effect of opioids.
The city will also expand public training on the recognition of opioid overdoses and the use of naloxone, advocate for wider access to buprenorphine, and provide more support for so-called “hot transfers” to treatment. addiction from health care, prisons and community settings.
Penn’s study was supported by grants from the U.S. Centers for Disease Control and Prevention and the Robert Wood Johnson Foundation.
[ad_2]
Source link