.jpg)
[ad_1]
A study by researchers in Germany found that the B.1.617 variant of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that emerged in India entered certain types of lung and intestinal cells with slightly increased efficiency. compared to the original. wild type strain.
The B.1.617 variant is the lineage believed to be responsible for the sharp increase in 2019 coronavirus disease (COVID-19) cases and deaths in India in recent weeks.
The team – from the German Primate Center in Göttingen, the Medical Center at the University of Göttingen, the Friedrich-Alexander University in Erlangen-Nürnberg and the Faculty of Medicine in Hanover – also reports that the entrance to B.1.617 in lung and intestinal cells was blocked after treatment. with soluble angiotensin converting enzyme 2 (ACE2) or serine protease inhibitor Camostat.
However, this entry into the host cell was not blocked by the monoclonal antibody Bamlanivimab, which has received emergency use authorization (EUA) as a COVID-19 treatment.
Finally, B.1.617 also partially eluded neutralization by antibodies induced by natural infection or immunization with the Pfizer-BioNTech BNT162b2 vaccine.
Markus Hoffmann and his colleagues say that the escape of antibodies by B.1.617 may contribute to the rapid spread of this variant.
A pre-printed version of the research paper is available on the bioRxiv* server, while the article is subject to peer review.
.jpg)
Emergence of variants threatens efforts to contain pandemic
Since the start of the COVID-19 epidemic in late December 2019, variants of the causative agent SARS-CoV-2 have emerged and threaten efforts to contain the pandemic.
For example, the B.1.1.7 line which emerged in the UK and is now spreading to many countries shows increased transmissibility compared to previously circulating strains.
Researchers suspect that this increased transmissibility may be linked to the N501Y mutation in the receptor binding domain (RBD) of the viral spike protein – the main structure the virus uses to infect host cells.
This spike protein is made up of two subunits. The RBD in subunit 1 binds to the ACE2 host cell receptor, which is followed by activation of the peak by serine transmembrane protease 2 (TMPRSS2) or other cellular proteases. The 2 (S2) subunit then facilitates the fusion of the virus and the cell membrane to allow delivery of the viral genome into the cell.
These processes are essential for SARS-CoV-2 infection, and the spike protein is the primary target of monoclonal antibody therapies and neutralizing antibodies generated as a result of vaccination or natural infection.
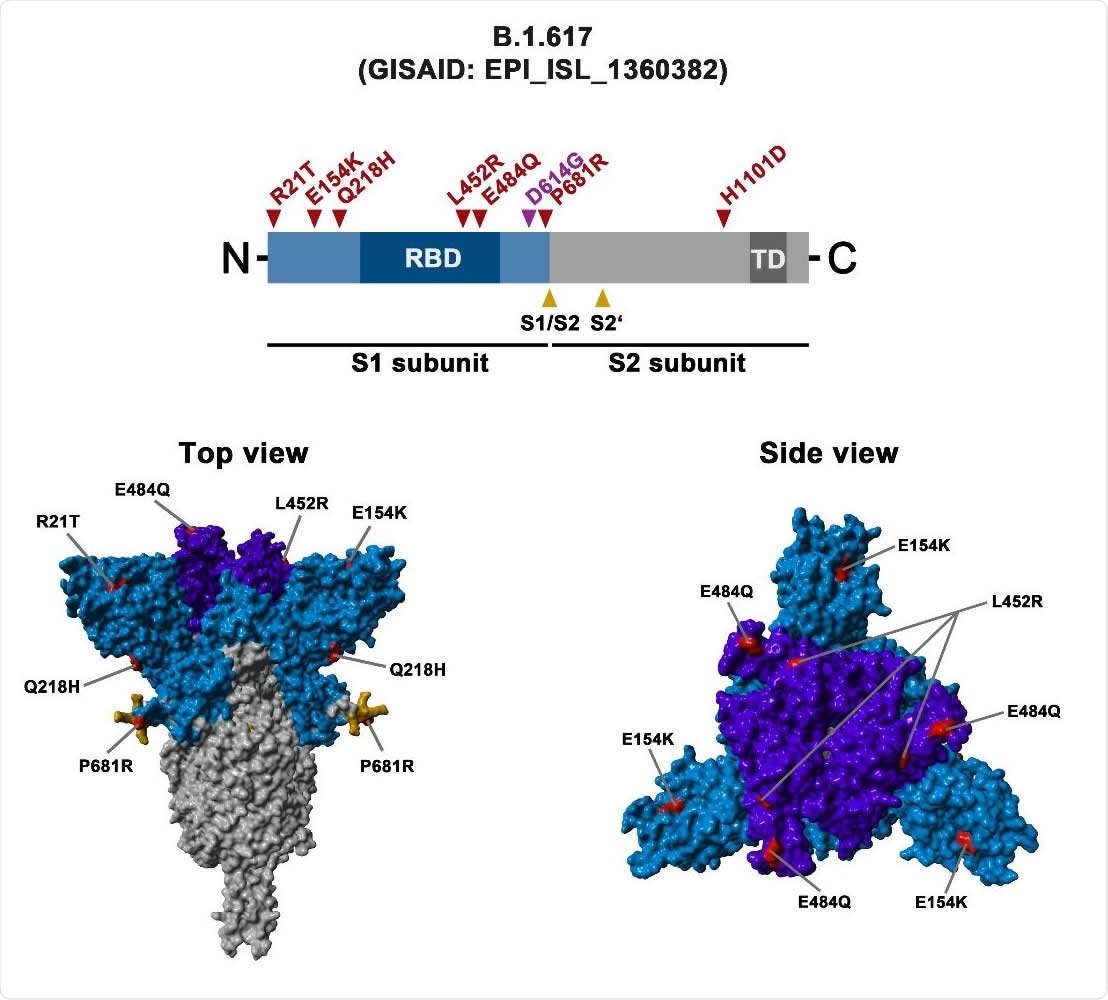
Schematic overview of the S protein of the B.1.617 variant of SARS-CoV-2 The localization of the mutations in the context of the organization of the B.1.617 S protein domain is shown in the upper panel. RBD, receptor binding domain; TD, transmembrane domain. The location of the mutations in the context of the trimeric S protein is shown in the lower panels. Color code: light blue, S1 subunit with RBD in dark blue; gray, S2 subunit; orange cleavage sites, S1 / S2 and S2 ‘; red mutated amino acid residues.
What about the other variants?
The B.1.351 and P.1 variants which became dominant in South Africa and Brazil, respectively, harbor the RBD E484K spike mutation, which has been shown to reduce neutralization by antibodies.
So far, antibody escape has been found to be the most important for the B.1.351 variant, however, it is not clear whether variants can appear which still exhibit additional or even complete resistance to the. neutralization.
The sharp rise in COVID-19 cases and deaths in India in recent weeks is believed to be due to the new variant B.1.617, which harbors eight mutations in the spike protein. These include the RBD L452R and E484Q mutations, which are known to modulate antibody-mediated neutralization.
However, the researchers say it is not currently known whether B.1.617 is resistant to this antibody-mediated neutralization.
The researchers say it’s also unclear whether these cutting edge mutations could alter important properties such as the efficiency of entry into the host cell or sensitivity to certain drugs.
What did the researchers do?
To test whether B.1.617 is more apt to enter cells, the researchers infected eight cell lines with pseudotyped viral particles expressing the spike protein from the original wild-type virus, the B.1.617 variant or the B.1.351 variant. .
Of the eight cell lines tested, the spikes of B.1.617 and B.1351 mediated entry into Calu-3 lung cells and Caco-2 colon cells with slightly increased efficiency compared to the original strain. .
“The SARS-CoV-2 B.1.617 spike protein allows moderately improved entry into certain cells of the respiratory and digestive tract,” explains Hoffman and colleagues.
Next, the researchers showed that this entry caused by peaks in B.1.617 could be inhibited by soluble ACE2, which targets RBD and blocks subsequent engagement of membrane-bound ACE2. Cell entry was also blocked by the serine protease inhibitor Camostat, which targets TMPRSS2.
“These results indicate that soluble ACE2 and Camostat will be active against the B.1617 variant,” the team writes.
Neutralization by monoclonal antibodies, convalescent and vaccinated sera was affected
In contrast, cellular entry of B.1.617 was partially resistant to neutralization by Casirivimab and fully resistant to neutralization by Bamlanivimab – two monoclonal antibodies that have received emergency use authorization as COVID-19 treatments.
“These results suggest that casirivimab and in particular Bamlanivimab as monotherapy may not be suitable for the treatment of patients infected with the B1.617 variant”, explain the researchers.
In addition, cell entry B.1.617 was partially resistant to neutralization by sera from convalescent individuals and sera from individuals immunized with two doses of Pfizer BNT162b2 vaccine.
Escape of antibodies by B.1.617 may contribute to its rapid spread
“The present study reveals that the spike protein B.1.617 can facilitate entry into Calu-3 and Caco-2 lung cells in the colon with slightly increased efficiency and shows that entry can be blocked by soluble ACE2 and Camostat Explains Hoffman and his colleagues.
“In contrast, Bamlanivimab, a recombinant antibody with EUA did not inhibit peak B.1.617-induced entry and evidence of moderate infection-induced escape of antibodies, and BNT162b2 vaccination was obtained” , they add.
Collectively, the study reveals that the escape of antibodies by B.1.617 may contribute to the rapid spread of this variant, the team concludes.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer reviewed and, therefore, should not be considered conclusive, guide clinical practice / health-related behaviors, or be treated as established information.
[ad_2]
Source link