
[ad_1]
We have recently heard a lot about Candida auris, a deadly, multidrug-resistant fungus emerging around the world. This pathogen has been labeled "new fungal superbug" and is a significant threat to public health.
C. auris tends to infect people whose immune systems are weakened or compromised. It develops on the skin where it persists for long periods.
It also penetrates into the patient's environment – usually a hospital or retirement home – and sticks very well to the surface.
In hospitals, invasive fungal infections, especially candidiasis caused by C. auris, can compromise patient safety and worsen outcomes after cancer treatment or surgery.
But it's hard to diagnose and, above all, to C. auris has a resistance profile that can make it very difficult to treat.
Many people who contract an infection caused by C. auris will not survive.
Read more:
A frenemy mushroom provides clues to a new mortal
How common is this deadly fungus?
C. auris has been identified for the first time in 2009 in Japan.
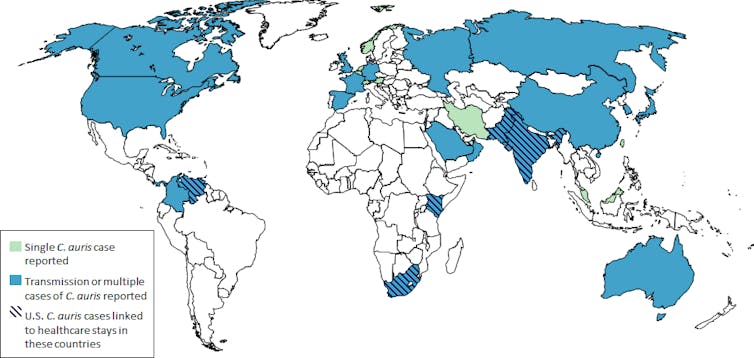
Infections have since been reported in several countries, but the prevalence of C. auris was probably underestimated in most places. Indeed, it is difficult to identify and monitoring programs, where they exist, may not take into account all cases.
The Centers for Disease Control and Prevention in the United States reports that 617 cases of C. auris have been detected in the United States.
CDC
Australia has had very few cases and the cases we have seen were mostly acquired abroad.
The Victoria State Department of Health has indicated that hospital stays in a number of affected areas, such as the United Kingdom, India, Pakistan, China , South Africa and parts of the United States, could pose a risk.
How does it manifest and how is it diagnosed?
C. auris seems to colonize and infect most often people already sick or whose immune system is compromised, for example cancer patients or transplanted, or hospitalized patients very young or very old.
Risk factors include suppression of the immune system (eg, medications after an organ transplant to prevent organ rejection), recent surgery, diabetes, and the presence of an immune system. internal medical device such as a catheter.
Read more:
A deadly mushroom has destroyed 90 species and threatens hundreds of others
The presence of the fungus on the body, called colonization, does not necessarily cause the disease.
But invasive candidiasis (that is, an invasive candida species) can infect blood circulation (candidemia), central nervous system and internal organs.
When the infection spreads in the blood, it can manifest as sepsis, accompanied by symptoms such as fever, rapid breathing, muscle aches and confusion.
Just like serious bacterial infections, C. auris can form abscesses in different parts of the body and require surgery.

From shutterstock.com
It can be difficult to diagnose fungal infections and accurately identify the species that caused the infection. C. auris is very similar to other common fungi of the candida kind and can be misidentified.
In most Australian hospitals, we use a blood culture diagnostic test. This is time consuming and involves specialists to accurately identify the pathogen.
Alternatives such as molecular diagnostic tests are not commonly used in many hospitals because of their cost and, even when they are, they may not be able to accurately identify the type of fungus that caused the infection.
However, these tests are improving and will be more widely available soon.
Results for people who contract C. auris
Patients with weakened immune systems who have candidemia or invasive candidiasis have a 30-60% chance of dying after being infected.
But it can be very difficult to tell if these patients die from their infection or die from their infection, the infection usually occurring when a person is already very sick.
Read more:
Explainer: why do we have nail fungal infections and how can we treat them?
Another problem is that treatment with antifungal drugs is systematically delayed. The time between taking a blood sample and delivering the test result often exceeds 48 hours, which can result in late or inappropriate treatment (because the cause of the infection is still unknown).
Delaying antifungal therapy is associated with an increased risk of death.
For these reasons, we need better tests to diagnose fungal infections.
Why resistance has developed
C. auris has developed resistance to several different antifungal medications.
While its resistance profile varies geographically, C. auris is almost universally resistant to fluconazole, a reliable drug of the class of azole antifungals – one of the four main classes of antifungals existing.
We need to know more about this, but it has been suggested that the prevalence of antifungal use in the environment contributes to the acceleration of resistance.
For example, in the presence of azole pesticides, we have seen the emergence of azole-resistant pesticides. Aspergillus, another kind of mushrooms. The resistant strains then reproduce in the soil and the infections can be contracted by the spores present in the inhaled air.
Similar processes may also have led to the emergence of resisters. C. aurisbut we do not know for sure.
Read more:
Five of the most scary bacteria resistant to antibiotics in the last five years
How can we control it?
C. auris is notoriously difficult to erase. This poses enormous problems for the cleaning of hospitals and the control of infections.
In addition to disinfectants with antifungal activity, hydrogen peroxide vapors or ultraviolet rays are also used, whenever possible, to clean up contaminated environments.
Australia is on full alert and hospitals are screening patients who may have been exposed.
But we need constant vigilance and coordinated efforts to stop its spread in hospitals and to diagnose it quickly. We must also use antifungal agents wisely in the field of human health and the environment.
This article has been updated to name Candida auris as "drug-resistant" rather than "antibiotic-resistant".
[ad_2]
Source link