[ad_1]
The war against bacteria and other microorganisms brings together hospitals, doctors, public authorities and the pharmaceutical industry in the same trench. With some microbes capable of surviving the most potent antibiotics ever created, it is feared that their infections will kill millions of people over the next few decades.
The problem is already haunting the present. According to estimates by the British government, 700,000 people die each year from infections and between 2015 and 2050, the number of deaths due to supermicrobial infections can reach 2.4 million alone, according to an estimate from the US. OECD. for economic co-operation and development.)
The cost of managing this rather catastrophic scenario would also be enormous, with an average of about 3.5 billion euros (annual average) for each member country of the organization. .
According to an American estimate, between 20% and 50% of antibiotic treatments practiced in this country are incorrect or unnecessary – in other words, the remedy is used for simpler cases that do not require any treatment. antibiotics or an incorrect remedy. is used to treat a particular infection.
In Brazil, there is still little data on the subject. Anvisa has monitored primary bloodstream infections in the ICUs of 1,900 hospitals in the country since 2010, but their numbers are far from representing the number of people with multidrug-resistant microbes.
Since the discovery of penicillin by Alexander Fleming 90 years ago, it was already known that certain microorganisms in nature were simply immune to certain antibiotics. This means that in their cellular machinery, these microbes have the means to degrade or simply to get rid of these aggressive molecules.
The problem takes on a dimension if one takes into account that these resistance strategies can be copied and shared between bacteria, generating multidrug-resistant organisms
In the end, antibiotics, when they are misused, destroy bacteria "more or less". Only the highly qualified and able to generate infections difficult or impossible to fight with the current pharmacological tools
Several sectors have concluded that it was necessary to rationalize the use of drugs
An example already Practical is that of Santa Casa de Santos, which, as a reference for the region in complex cases, consumes a lot of antibiotics. However, it is known that the hospital environment is one of the most favorable for multidrug-resistant infections, thanks to the confluence of patients.
A strategy adopted at the hospital attempted to reduce the time of hospitalization of patients. "They ended up being hospitalized for a long time to use antibiotics, but the hospital environment is risky.We know that a person risks his life more by entering a hospital than by plane," says Priscilla Sartori, director of pharmacy, responsible for the management of antibiotics (or management).) Of the hospital.
The city hall, partner of the initiative, applies drugs at home in case In some cases, the patient was able to stay 80 days less at the hospital, reports Sartori, but you have to be careful: "The exit from the hospital is not an outlet for medical care. Dehospitalization must be done with quality. If this happens, home recovery is much faster. "
In return for the initiative launched in 2017, more than a thousand days of resuscitation have been saved, thus opening up jobs for those who need it most." The management of antibiotics poses particular problems for each country Ana Gales, coordinator of the Antimicrobial Resistance Committee of the Brazilian Society of Infectious Diseases and a professor at Unifesp, said that isolated initiatives had existed for several decades, but that more coordinated efforts had begun to emerge, including in Europe, in the United States and in other countries such as Canada and Australia
"I must inform the clinical staff of the microbiological reality of this hospital, what is the best therapeutic option for patients, which is different from Oswaldo Cruz Hospital, Hospital das Clínicas of the USP and even more different from any American hospital ", expl He is the infectiologist Pedro Mathiasi, who is coordinating the HCor management program in São Paulo for three years.
He explains that every six months or a year is necessary to make an inventory of the pathogens present in the hospital and to discover the resistance profile. Thus, it is possible to discover valuable data such as the fact that 25% of bacteria in the region are resistant to the antibiotic quinolone – a drug widely used to treat urinary tract infections. In this way, it is possible to choose another drug more suitable to solve the problem
The use of antibiotics in the hospital dropped by about 20%; the use of antifungals also decreased by 25%. In pediatric intensive care, the reduction has reached 60%. In addition to the reduced cost, there is less risk of side effects for those treated in this more rational way.
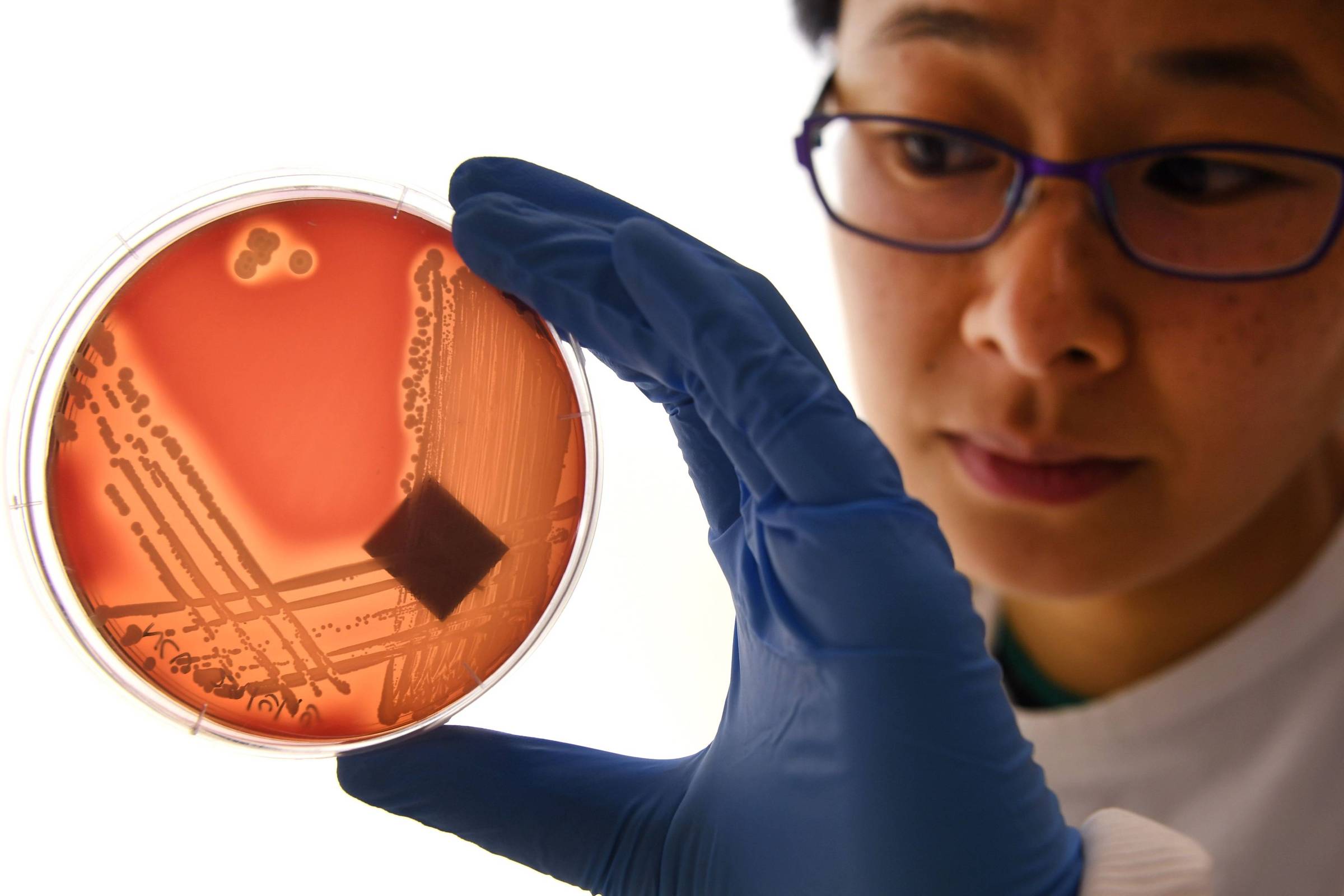
Both Santa Casa de Santos and HCor were supported by the pharmaceutical MSD, which helped hospitals implement their management programs. including supporting the establishment of microbiology laboratories – where pathogens can be identified, as well as the antibiotics to which they are resistant.
Following sectoral initiatives, Brazil launched last December a multi-ministerial program for the fight against pathogens. (Ministry of the Environment, Health, Agriculture and Science and Technology, among others), outlining a strategy that includes health education, the promotion of human and animal hygiene, and the monitoring of health to ensure:
Also in December, Anvisa published rules on how to interpret tests. antibiotic sensitivity for choosing the best treatment. The guideline is to use the lightest possible strategy to kill microorganisms
Another measure, already in force, is the maintenance of pharmacy prescription in order to limit the indiscriminate use of drugs. Antibiotics
. The most ignored question, according to Anne Welsh, is the use of antibiotics in animals. "Animals get bigger and have fewer infections, and this inappropriate use in the diet to promote growth is even worse because it occurs as a sub-dose, which further favors the selection of these resistant bacteria."
Infectiologist indicates that some simple measures can be used by the population to prevent infections by multidrug-resistant organisms. The first is to avoid unnecessary visits to the hospital. If you have to go, it is advisable to wash your hands very well.
Another forgotten recommendation is to get vaccinated. Adults should also keep their vaccination records up-to-date to avoid diseases such as tetanus, pneumonia and yellow fever.
Discovery of some of the major antibiotics
1909 Salvarsan (Arsphenamine)
A synthetic compound was able to treat syphilis effectively for the first time
1928 Penicillin [19659026] First broad-spectrum antibiotic for the treatment of serious streptococcal and staphylococcal infections
1943 Streptomycin
It marked the beginning of the golden age of antibiotics. This was the first treatment against tuberculosis
1953 Vancomycin
] One of the most effective antibiotics; resistant bacteria did not appear until after three decades
1962 Quinolones
Used in some cases of urinary tract infection, they can have serious debilitating effects
1976 Carbapenems
Still relatively effective, the Last resort to treat many infections
1987 Daptomycin
One of the last clbades of antibiotics discovered
Source link